Hysterosalpingogram (HSG) is performed less commonly in modern gynecology than in the past, but it is still a valuable tool for some patients. A well performed HSG should be relatively painless and its results need to be correctly interpreted in context of what is already known about the patient. Here are four tips for performing an HSG.
1. Use a catheter.
Use a modern HSG catheter with an inflatable balloon tip rather than a reusable Cohen intrauterine cannula. Disposable catheters with a balloon can be purchased for about $15 or less and allow for the procedure to be performed with much less pain and discomfort than a traditional reusable cannula which requires a tenaculum to be placed on the cervix and instrumentation of the cervical canal in many cases. The balloon catheters are also more versatile in that they can be floated to different parts of the cavity or even placed intracervically (see Tip #4).
2. Beware of the false positives.
One of the most common reasons for an HSG today is to check for tubal patency. Office-based saline-infusion sonography (SIS), especially when combined with a 3D reconstruction, is very effective for providing views of the uterus and cavity and this study (so-called virtual hysteroscopy) has essentially replaced HSG for exploring uterine malformations, Asherman Syndrome, etc.
Thus, HSG today is commonly used to check for tubal occlusion following an Essure sterilization or to check for tubal patency as part of a workup of infertility. How accurate the test is will vary based upon the pretest probability of tubal occlusion for a given patient. Swart et al. determined that the point sensitivity for HSG (compared to chromopertubation) was 0.65 with a specificity of 0.83 for tubal blockage. Consider three patient situations:
- A woman with secondary infertility (who has a 0.29 risk of a blocked tube)
- A woman who is status post Essure sterilization with two coils visualized in the correct anatomic location on fluoroscopy (who has a 0.99 risk of a blocked tubes)
- A random woman (who has about a 0.03 risk of a blocked tube)
Using the above sensitivity and specificity, the following positive and negative predictive values would be calculated:
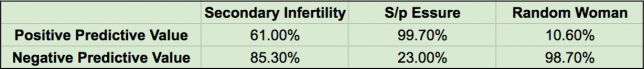 These numbers are very important and highlight one of the leading problems in clinical medicine: Incorrect diagnoses often occur because the pretest probability isn’t considered when determining predictive values of the test. If the patient has had an Essure and both coils are visualized in the appropriate location, then despite the rather high rate of tubal spasm that can occur with an HSG (about 1/3), the positive predictive value is still on the order of 99.7%. On the other hand, if the patient is being evaluated for secondary infertility and the test shows a blocked tube, the positive predictive value is only 61% (as compared to the gold standard of chromopertubation).
These numbers are very important and highlight one of the leading problems in clinical medicine: Incorrect diagnoses often occur because the pretest probability isn’t considered when determining predictive values of the test. If the patient has had an Essure and both coils are visualized in the appropriate location, then despite the rather high rate of tubal spasm that can occur with an HSG (about 1/3), the positive predictive value is still on the order of 99.7%. On the other hand, if the patient is being evaluated for secondary infertility and the test shows a blocked tube, the positive predictive value is only 61% (as compared to the gold standard of chromopertubation).
The real trouble happens when an HSG is done on an average, random woman who has nothing that would elevate her pretest probability for tubal occlusion. In this case, the result of blocked tube on HSG would carry only a 10.6% chance of actual tubal occlusion. Most of the apparent blocked tubes are the result of tubal or cornual spasm rather than true pathology. This statistic is particularly important as FemVue becomes more common in office practice.
FemVue (an agitated saline-infusion device) is used with ultrasound to test tubal patency in the office. It performs roughly as well as HSG when compared to chromopertubation in terms of sensitivity and specificity. The problem is that its use has been expanded in many cases to an inappropriate patient population. For example, some clinics perform it routinely on all fertility patients even if they have another underlying cause of infertility already established (like anovulation). In this case, the pretest probability of tubal occlusion (assume the woman has no history of chlamydia, etc.) is similar to that of a random woman. When tubal occlusion is noted on FemVue in a patient like this, the positive predictive value is close to 10%. So, in some populations, about 90% of positive results are false positives. This is a dangerous consequence of indication drift and a poor understanding of the role that pretest probability plays in determining the predictive value of a test.
3. Low pressure or high?
There are two somewhat different goals of HSG: to test the patency of the fallopian tubes and to visualize the contours of the cavity. Higher pressure of the contrast medium helps distend the walls of the uterus but is also more likely to cause tubal or cornual spasm, leading to a false positive result. So, a low pressure technique is more effective if the primary aim is to test the patency of the tubes, which is the most common objective of HSG. Inject the contrast medium at a slow and steady pressure and you shouldn’t need more than 2 or maybe 3 ml for the whole study. If the patient reports significant cramping, you are probably using a too much pressure (and that cramping may be associated with tubal spasm).
4. Try putting the balloon in the cervix.
Sometimes due to the acuteness of the uterocervical angle, the flexible catheter cannot pass easily into the endometrial cavity. Other times, the views of the cavity are incomplete because the tip of the catheter (and the balloon) are situated in the cornua and the contrast doesn’t distend the rest of the cavity well. Or, sometimes, the cavity won’t distend well because the contrast is leaking of the cervix.
In each of these cases, try this: place the catheter balloon in the cervix rather than the endometrial cavity, near the internal os, and inflate it. This will put the tip of the catheter in the lower uterine segment and the inflated balloon will occlude the cervical canal enough to force the contrast material upwards. This usually works and can make using a painful tenaculum unnecessary (either to pull on and straighten out the uterocervical angle or to try to occlude the cervical canal).
What else?
Use oil-based contrast instead of water-based contrast in infertility patients. Oil-based contrast is associated with a higher pregnancy rate. Beware of false positives associated with intravasation of contrast media into the parametrial vasculature. Do the test early in the follicular phase, particularly for fertility patients, to make sure that there isn’t an early, luteal-phase pregnancy.
Check out the video below for the basic technique:

