I’ve attended two conferences in the last 3 weeks that largely revolved around maternal mortality in the United States. About 700 women each year die in the United States during or around the time they give birth. For those of who practice Obstetrics, we believe that even one is too many. I’ve been reading and writing about maternal mortality for years and here are ten thoughts about the problem that I’ve had in the last three weeks.
1. US maternal mortality isn’t as bad as it seems.
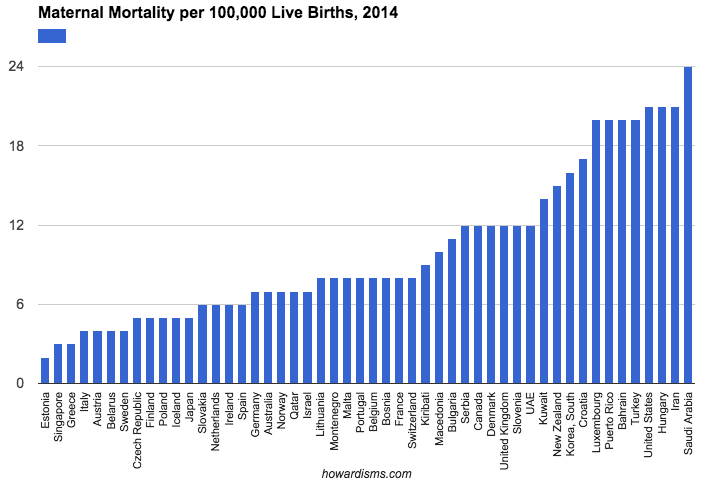
Wait … what? Then why is it getting so much attention? Let me explain. As I sat through various meetings and conferences, many speakers started their sessions by comparing US maternal mortality rates to other countries in the world. When you do that, we look bad for sure.
This graph is from my article The Percentile Fallacy that discusses some of the issue related to comparing our maternal mortality rate to that of other countries. Notice that the US is 47th in this list of countries, behind places you wouldn’t expect to have lower maternal mortality rates than us.
The sometimes stated but often implied accusation is that the US spends so much money on maternal care yet comes up dramatically short. But this simply isn’t true. I cringe every time someone brings this up because I think most of them know better. We calculate our maternal mortality rates in a significantly different way than virtually every other country in the world. The numbers are simply not comparable. The best way to have a low maternal mortality rate (on paper) is to do poor data collection and limit maternal mortality deaths to those directly attributable to the pregnancy (e.g, not counting deaths in car accidents that occur while pregnant).
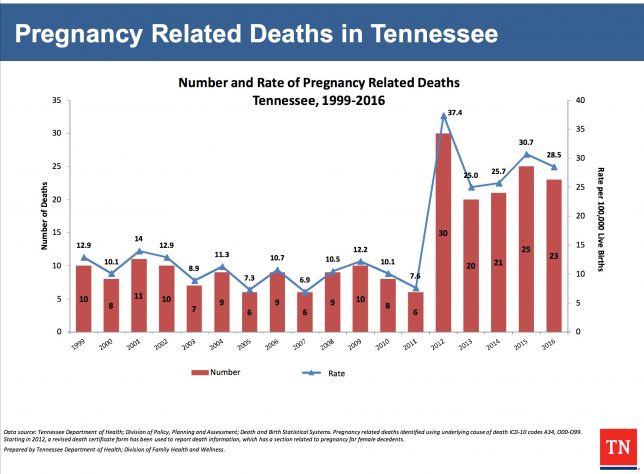
Even in the US, we have seen that just changing the way we collect our data has dramatically changed the numbers. In Tennessee, the rate of maternal mortality in 2011 was 7.6; one year later it was 37.4! What happened? Did we all of a sudden forget how to take care of pregnant women? No. We changed how we collect the data. If we have so much difficulty knowing what our own true maternal mortality rate is in the US and if data collection can make such a dramatic impact on the numbers, then is it any wonder that the Czech Republic might have 1/3 the maternal mortality rate that we do? They don’t in reality; they just collect data differently. So we need to stop with the fruitless international comparisons. That being said…
2. US maternal mortality is bad and it’s getting worse.
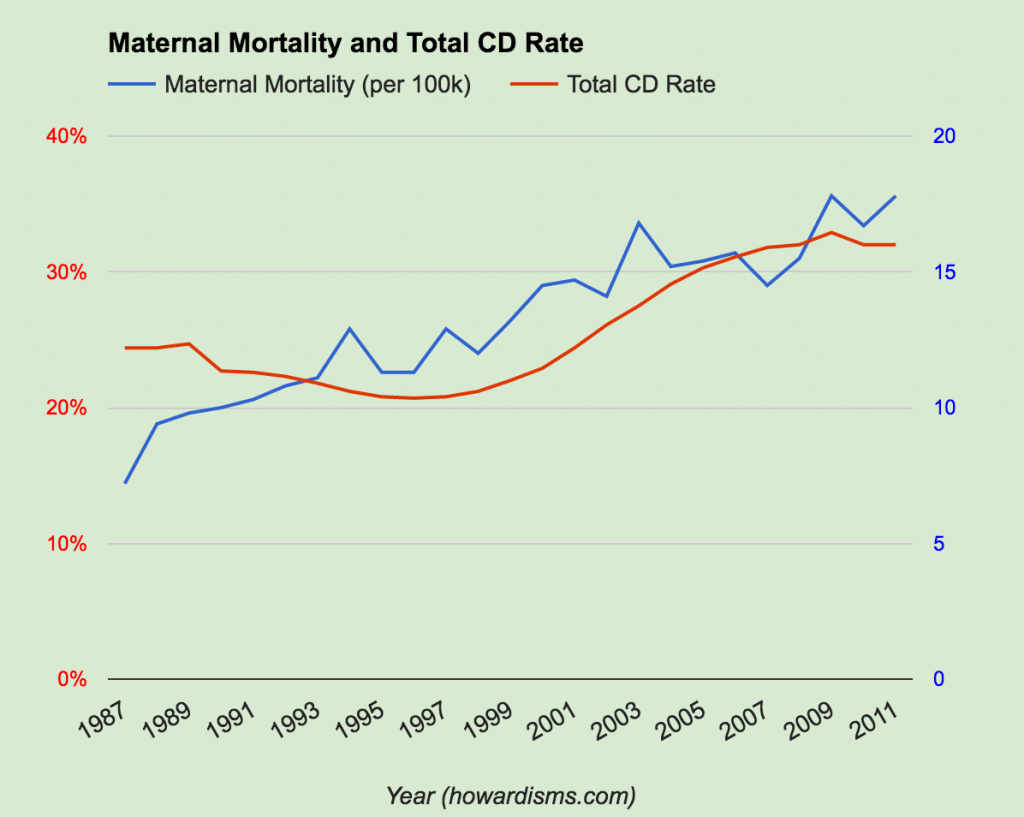
What we can do with our data is compare the US maternal mortality rate this year to the US rate in previous years. When we do, we see a disturbing trend: maternal mortality is increasing. One of the plusses of not radically changing the way we have collected data over many decades is that we can compare where we are in the US now to where we used to be and understand if we are making progress or falling behind. Look at this chart from my article Historic Decline in Maternal Mortality (worth the read by the way):
We made tremendous strides in lowering maternal mortality up until about 1987. In 1840, the rate was has high as 1500/100,000; by 1987 Obstetricians had lowered that rate to around 8/100,000. Since then, however, it has gone up to as high as 23.8/100,000 in 2014! This is clearly a change in our rate and it is unacceptable.
3. We don’t really know why maternal mortality has worsened.
Why has maternal mortality increased? Some of it is undoubtedly due to better data collection. In the past, at the left side of the graph above, women primarily died due to:
- Infection
- Hemorrhage
- Toxemia (eclampsia, etc.)
- Embolism
Today, the causes have changed. In Tennessee, in 2016, the leading causes were:
- Accidents (37%)
- Intrapartum pregnancy causes (22%)
- Hemorrhage, preeclampsia, amniotic fluid embolism, pulmonary embolism, ectopic pregnancy, infection, etc.
- Assault (7%)
- Cancer (5%)
- Suicide (5%)
- Heart disease (4%)
- Respiratory diseases (1%)
- Congenital malformations (1%)
- “Other” (18%)
This list varies some state by state, but it doesn’t tell the whole story. We think that perhaps as many as 60% of these deaths were preventable. But what are the real underlying causes? What has changed?
- An increase in opioid abuse is associated with more accidents, suicides, and assaults.
- An older and more obese patient population is associated with more underlying medical conditions, a higher risk of Cesarean, a greater risk of pulmonary embolism, hemorrhage, and amniotic embolism, and a greater risk of infection.
- A changing demographic (as non-white, non-Asian women suffer dramatically higher rates of maternal mortality than their white or Asian counterparts).
- An increase in the rate of depression among American females (which is at an all-time high).
- Less continuity of care with pregnant women and their physicians.
- An increased rate of Cesarean delivery (due to a variety of causes, e.g., more defensive medicine, etc.).
- Lots of scarred uteruses due to the high Cesarean rate are associated with the highest number of cases of invasive placental disease ever (and the accompanying rates of hemorrhage and severe surgical risks that go with it).
All that being said, we really don’t know enough to pin down specific changes/causes and the magnitude of effect each might have. However, we do know that many of these causes of death are preventible and that we were doing a better job of preventing maternal mortality 30 years ago than we are today.
4. Cesareans don’t get enough attention in the conversation.
Every time I read anything new about maternal mortality or go to a conference or working group, I almost never read or hear anything about the rising Cesarean delivery rate. Many states that have Maternal Mortality Review Committees (MMRCs) do not consider deaths that follow a Cesarean as preventable. It seems that the assumption is that no Obstetrician alive has every done an unnecessary Cesarean (or done with poor technique). No one wants to have this conversation. But … we know that the risk of a woman dying after Cesarean increases 4-7 fold as compared to a vaginal delivery. Almost every case of maternal mortality I hear about or have seen involved a Cesarean delivery. I’m confident that some of those Cesareans were unnecessary and that the best techniques weren’t always used.
Look at this graph from my article To Induce or Not To Induce: The 39 Weeks “Debate”:
There is clearly an association between the rising rate of Cesarean and the rising rate of maternal mortality. We cannot continue to act like Cesarean delivery is as safe as vaginal delivery. We also cannot act like our current rate of Cesarean is appropriate or acceptable. Lowering the rate of Cesarean delivery would go along way towards reducing our maternal mortality rate. Read how to do that here.
5. “An ounce of prevention is worth a pound of cure.”
Ben Franklin was right. We need to focus more on how to prevent mothers from getting so sick to begin with rather than focus on better techniques for critical care once they are already sick. Granted, both are important to consider, but it’s prevention severely-sick mothers that has made the difference historically.
Consider third world countries that have high maternal mortality rates, like Sierra Leone or Niger. Those countries and many other sub-Saharan African countries have maternal mortality rates comparable to what the US experienced a 100+ years ago. In fact, hundreds of women die each week in Africa due to hemorrhage and hypertensive disorders (both accounting for nearly as many maternal deaths in a week as the US experiences in a year). We have largely eliminated these problems in the US not with expert ICU care or ECMO and blood banks, but by prevention. We check blood pressures regularly and induce women with event a hint of hypertension before they get critically ill (saving hundreds of lives per week nationally). We give women prophylactic oxytocin and actively manage the third stage of labor to prevent hemorrhage (also saving hundreds of live per year). We rub the uterine fundus of newly delivered women every 15 minutes after birth. We (try to) give pregnant women flu vaccines. We offer safe and effective birth control and sterilization to prevent pregnancies in at-risk women.
I could go on.
But, the point is that we need to think prevention: How can we prevent maternal deaths to begin with, not just do a better job of critical care? This type of thinking encourages root cause analyses. For example, if a mother dies of a pulmonary embolism after a Cesarean delivery, then we need to focus not just on whether she had risk factors that might have necessitated prophylactic anticoagulation, but also on why she had the Cesarean to begin with. Perhaps she was induced in her first pregnancy at 37 weeks after a BPP showed an AFI of 4.8; and perhaps this BPP was performed only because she was 36 years old. If these are the circumstances, then what really killed her was the unnecessary BPP, its incorrect interpretation, and probably poor decisions about the way the induction was conducted. Knowing root causes allows us to make the biggest difference in outcomes.
6. For every woman who dies, 70 have near death experiences.
Our emphasis on maternal mortality sometimes is ignored by policy makers when they realize that only 700 women out of over 4,000,000 die each year in the US. What’s more, only perhaps half of those deaths are theoretically preventable. So it’s tough to encourage Congress or others to invest in expensive programs that under the best circumstances might only prevent 350 deaths per year. But for every woman who dies each year, about 70 come close to death. In other words, don’t focus on the 700 but focus instead on the nearly 50,000 each year who almost die in childbirth. The fact that only 700 of the 50,000 die is a testament to the quality of our critical care abilities – and the availability of things like blood banks, super strong antibiotics, and state of the art ICUs. The care for those 50,000 women is expensive and scary. By focusing on prevention of maternal mortality (and morbidity), we stand to save a lot of money and pain for a lot of women.
Here’s another way of thinking about it: those 50,000 women represent about 1,000 women per week in the US. In Africa, those women would just die (and they are dying at that scale). In the US, we are saving most of their lives. But we can and must do more.
7. Most of the deaths and near-death experiences are preventable.
We don’t know for sure how many are preventable, but we know it is a lot. I suspect that if 50-60% of maternal deaths are preventable, even more near-misses are preventable. Why? Most of the unpreventable maternal deaths are caused by unforeseeable causes that have few, good treatments: things like amniotic fluid embolism, accidents, assaults, and cancers. But the preventable causes of maternal death make up the bulk of the causes of severe maternal morbidity: things like infection, hemorrhage, preeclampsia/eclampsia, etc. So while we might only save 350-400 deaths at most, I suspect we can prevent up to 40,000 cases of severe maternal morbidity with reasonable interventions.
8. We know that specific interventions can work to reduce maternal mortality.
So how do we do it?
The AIM Program is developing evidence-based protocols that should help and have already been shown to reduce maternal mortality in California and in other states where some of the bundles have been adopted. As of today, safety bundle exist for:
- Maternal hemorrhage
- Thromboembolism
- Opioid use disorder
- Reduction of primary Cesarean
A big part of reducing primary Cesarean is adoption of modern labor guidelines and performance of fewer inductions. More evidence-based induction protocols also will help. But we also need to emphasize the safety of vaginal birth after cesarean in order to make a real dent in the total number of cesareans and, consequently, maternal mortality.
Also, how about an environment that doesn’t marginalize the therapeutic benefit of antidepressants among pregnant women? Suicide in the first year after giving birth is a bigger problem than heart disease, but the same provider who would think nothing of giving appropriate treatment to a patient with postpartum cardiomyopathy often shies away from effective treatment of peripartum or postpartum depression.
Opioid abuse is a growing and complex problem. This issue is a common theme among deaths caused by accidents, suicides, homicides, infections, heart disease, and other maternal health conditions that lead to morbidity and mortality. It is also associated with less prenatal care, more shaming by providers (which tends to discourage access to care), and a fewer resources for care of the postpartum mother.
We do see a more obese patient population and a slightly older patient population than ever before. No one has a magic bullet for reducing obesity, but severely obese women planning a pregnancy should not be discourage from weight loss surgeries or other effective interventions preconceptually. We need more preconceptual care in general so that health conditions are optimally managed prior to conception. More preconceptual care opportunities comes from increased utilization of long-acting reversible contraceptives. What all can be accomplished? Smoking cessation, addiction management, weight and blood pressure management, diabetes optimization, encouragement of fitness activities and exercise, optimal folate supplementation, etc. immediately come to mind.
9. Physicians need to take more responsibility for the problems.
When any crisis exists, everyone likes to blame someone else. One thing that strikes me when I read about these problems is that no one really talks about what they can do better, but, rather, what others can do better or what the government can do for us all. But, let’s be clear about a few things that physicians have direct control over which contribute to excess maternal morbidity and mortality:
- Induction rates are higher than ever.
- Cesarean rates are higher than ever.
- VBAC rates are at a 30 year low.
- Unnecessary antenatal testing is at an all-time high.
- Opioid use is an epidemic (remember all those prescriptions for 30 Percocet after a vaginal delivery? That’s how it starts).
- Women’s mental health needs are neglected.
- Modern labor management guidelines are not followed by the majority of obstetric providers.
- Evidence-based techniques for things like Cesarean delivery technique, management of the third stage of labor, management of postpartum hemorrhage, induction of labor, etc. are usually not followed in clinical practice.
- Flu-shots and other appropriate vaccines are only tacitly recommended by far too many providers.
- Women who are underinsured are often discriminated against by practices and denied access to care.
These are not trivial things, and the list is incomplete. None of us need a grant from the Federal Government or a new law to tackle these issues. But, we must look carefully at our own practices and practice-patterns. Are you doing the best you can do? What is your primary and total Cesarean delivery rate? Do you take Medicaid? Do you prescribe narcotics for vaginal deliveries? Do you utilize SSRIs in pregnant women? Do you follow current labor guidelines? Do the majority of your patients get flu shots? Have you implemented hemorrhage protocols in your facility? Do you induce patients with unfavorable cervices without a medical indication? When you do an induction, do you use best practices for cervical ripening (foley bulb+pitocin or +misoprostol)? Do you over-utilize interventions like ultrasound? When you do a Cesarean, do you use best surgical techniques? Do you encourage VBAC candidates to try to VBAC? Do you encourage external cephalic version? Do you even check for presentation at 36-37 weeks? Do you transfer high-risk patients to a facility with the appropriate level of care? I could go on.
I encourage you to read The Serena Syndrome to understand how small things lead to bad outcomes.
10. Physicians who are involved with severe maternal morbidity or maternal mortality are probably not the best folks to determine what went wrong.
We can all work harder at implementing best practices with our own patients. However, when a patient does die, we are probably not the best ones to decide what happened. I’ve rarely ever met a person who could perform a quality root cause analysis on her own bad case. This is why we must have Maternal Mortality Review Committees in every state. One of the reasons why we don’t really know what has led to increased rates of maternal mortality is that there often is an unclear presentation of what went wrong and what could have been done better by the local team taking care of the patient. They hesitate to say anything could have been done better because it both helps them sleep better at night and also makes them feel like they have less liability exposure. But if 60+% of maternal morbidity is preventable, we need to know exactly where the breakdown occurred in order to design protocols to prevent the bad outcomes in the future.