Before we start, I’ll tell you that I don’t know what the ideal rate of Cesarean delivery should be; this is, at best, a controversial area of speculation. But I do think we can discuss some ideas that should inform the solution and come up with a credible range of answers.
Let’s consider some basic questions.
Does any woman ever need a Cesarean?
Yes. But, surprisingly, this fact is challenged constantly. For many women who believe that birth is and should always be an entirely natural process, all Cesareans (or at least almost all of them) are viewed as unnecessary or at least as the result of interventions that cause the need to arise.
Cesarean deliveries are done almost exclusively to benefit the health and safety of the baby, not the mother, though the mother may benefit too, especially when we consider how dangerous giving birth used to be. It’s hard to know exactly how many children used to die during birth itself since older records use conflicting terms. The word stillbirth was historically used to indicate a child that either was not born alive or did not live very long after birth; but records of stillbirth likely under-represent the number of children who died due to the birth process. At the same time, many fetal demises were due to problems we only rarely encounter today like hydrops fetalis (largely prevented with Rhogham) or any of a number of congenital infections (rubella, CMV, listeria, etc). Still, the chart below of rates of “stillbirths” from 11 developed countries can give us some idea of how many children didn’t survive being born in the era before modern obstetrics (and Cesarean delivery):
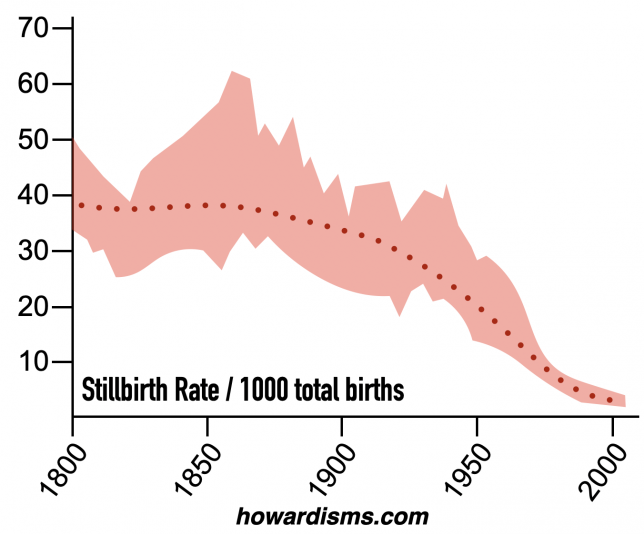
To put this in more relatable terms, it appears that roughly 4% of babies didn’t survive birth in 1850, either because they died before, during, or shortly after birth. Total infant mortality in 1850 (death before age 1) was around 20% while around 35% of children didn’t make it past age 5. Most of these later deaths were related to infections but some were due to lingering effects of birth trauma. So we might estimate that about 5% of children were ultimately lost due to something going wrong during the birth or pregnancy itself. Note that prematurity doesn’t likely account for too many of these deaths due to the way records were kept but it does definitely account for some of them.
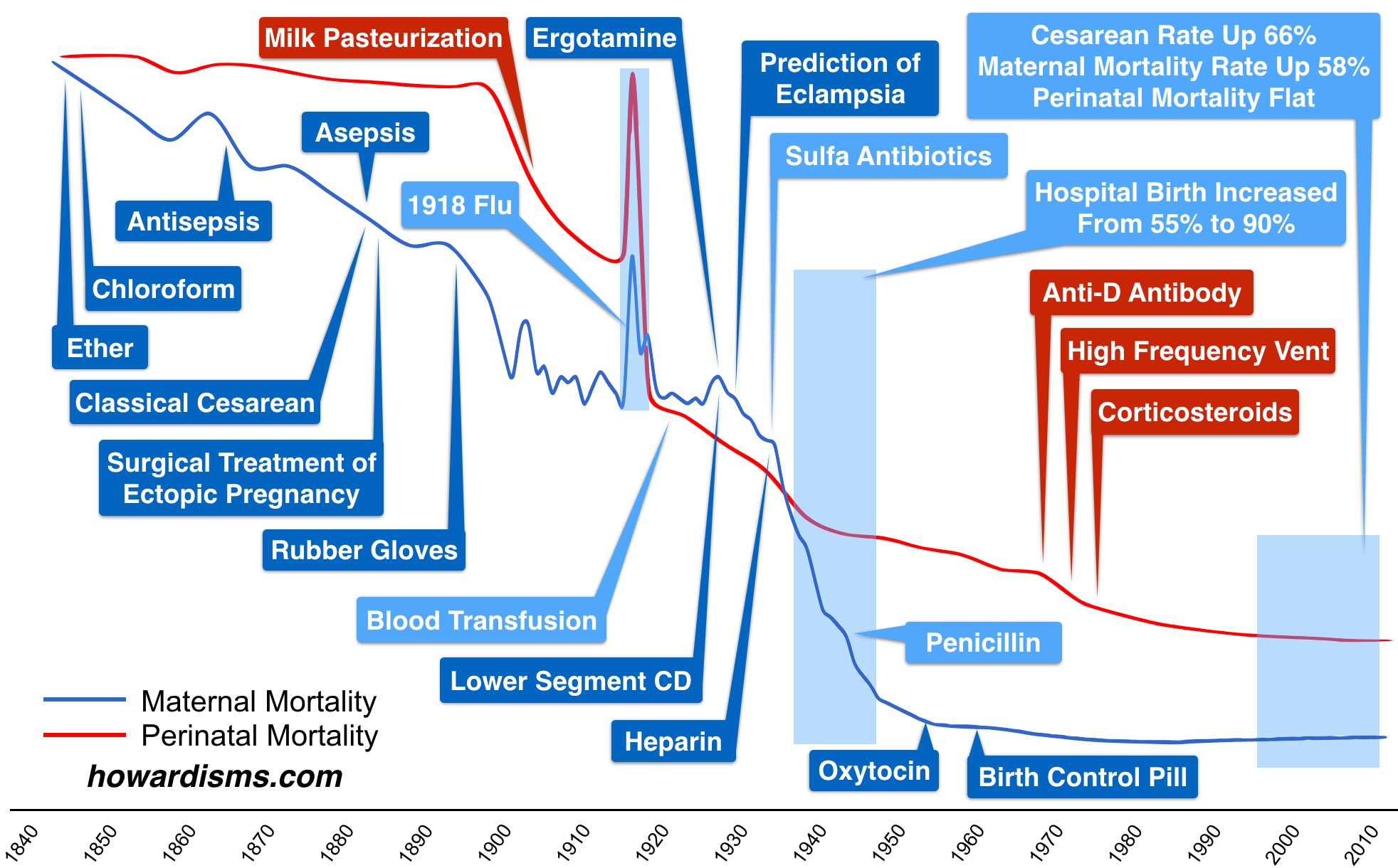
Numbers this high are unthinkable today and the reductions in these horrific rates of death are due to numerous factors with Cesarean delivery being only one of many. Oxytocin, antibiotics, Rhogam, and countless pediatric innovations have made a big difference. Still, safe Cesarean delivery is undoubtedly a huge factor.
Here are some of the other important innovations that have contributed over time to lower maternal and perinatal mortality:
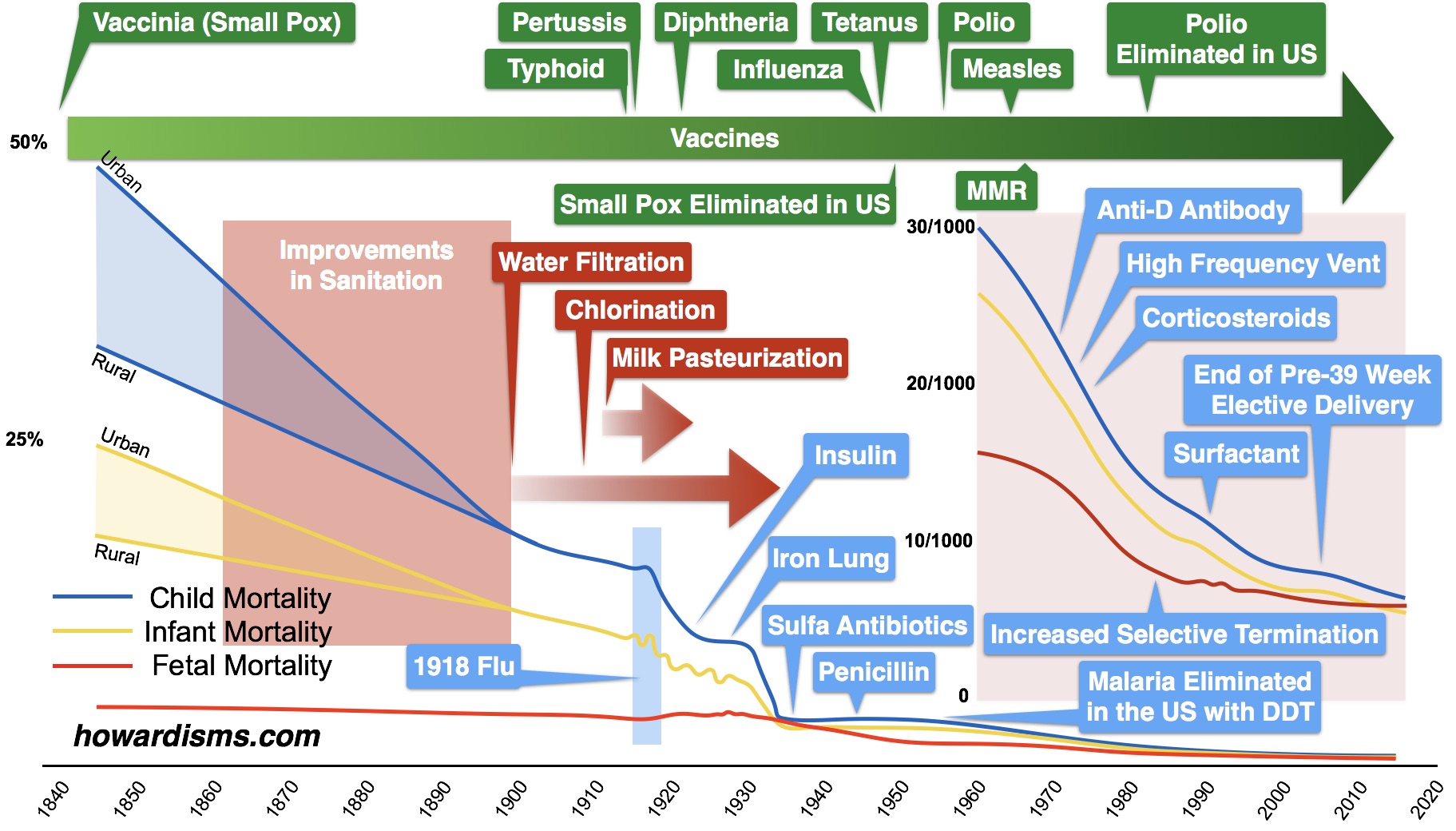
And child and infant mortality similarly have declined for a variety of reasons:
So estimating how much of a difference Cesarean delivery makes is difficult. Here are some situations where abdominal delivery can be imminently life-saving for an infant:
- Placenta previa
- Vasa previa
- Prolapsed umbilical cord (without complete cervical dilation)
- Significant placental abruption (perhaps greater than 20%) remote from delivery
- True fetal distress
- True cephalopelvic disproportion (very large babies or very contracted pelves)
- Uterine rupture
For each of these indications, there is a high probability that failure to do an abdominal delivery will result in fetal/neonatal death or disability. There are also many more indications for Cesarean where both short-term and long-term risks to the baby can be greatly decreased, like active genital herpes or maternal HIV with a high viral load.
So what percentage of Cesareans are truly life-saving? Well, it’s not the 5% that we discussed above. The absolute indications for Cesarean delivery are not very common. The clinical scenarios I just listed are not that common. But I do think it’s reasonable to estimate that 1-2% of children would die if not for Cesarean delivery. But, of course, that doesn’t mean that we can have a Cesarean delivery rate of only 1-2% since we don’t know with certainty in any given clinical scenario which babies are at no risk if vaginal delivery were allowed to proceed. This is particularly true for some of the fetal heart tracing abnormalities that lead to Cesareans.
Older obstetrics textbooks rarely reported or focused on fetal/neonatal death; they were instead most concerned with maternal mortality. However, The Place of Version in Obstetrics by Irving Potter from 1922 reports Dr. Potter’s individual outcomes from over 1100 births. He also reports that he had an 8% Cesarean delivery rate which means that he was a consultant for other difficult cases from general practitioners and midwives, so the numbers are inflated. Still, he brags in the book that he only had a perinatal death rate of 2.3%! Can you imagine if any doctor, in any population of patients, had a 2.3% loss rate during delivery? I grant that this was in a higher risk population of patients than average, but clearly we are not losing this number of newborns today.
The bottom line is that some number of Cesareans are necessary unless we accept an unnecessarily high rate of fetal/neonatal mortality. Cesarean delivery also is clearly associated with a lower risk of maternal mortality and morbidity, as well, compared to 150 years ago. Even though, generally, a Cesarean is more likely to kill or cause problems for a mother compared to vaginal delivery, in some specific cases it is clearly safer for the mother to have an abdominal delivery. In 1850, it wasn’t uncommon for women to labor for days with a baby that she couldn’t deliver vaginally and subsequently die of infection, for example. Still, today, at a time that we are doing too many Cesareans, this is now contributing to recent increases in the rate of maternal mortality.
What are the rates of Cesarean delivery in other parts of the world?
The United States often gets a bad rep in regards to maternal mortality, perinatal mortality, and its Cesarean delivery rate. Most of that bad reputation is based upon how we track data and I’ve written about that at length elsewhere. But we can compare our Cesarean delivery rate to other countries around the world and get a rough idea of how we match up.
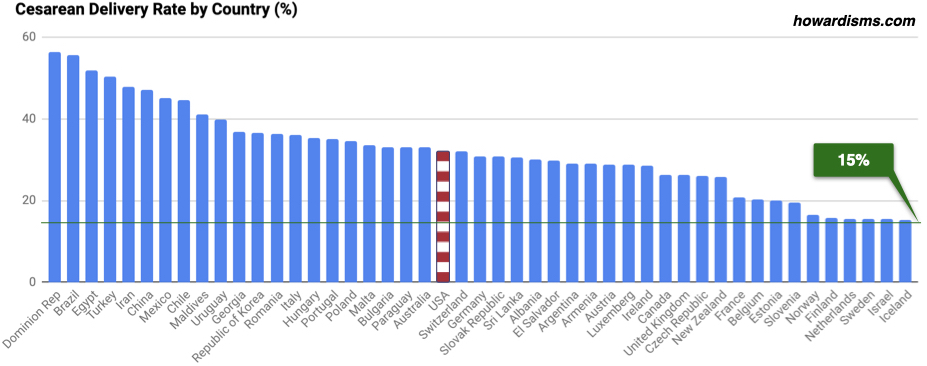
Clearly many highly-developed countries have much lower Cesarean rates than does the United States. Several countries to the right of this chart hover around 15%. The question then might be, do countries with low Cesarean delivery rates have higher perinatal or maternal mortality rates? In other words, does the lower rate of Cesarean delivery in those countries lead to harm?
The chart below shows maternal mortality in many of the same countries:
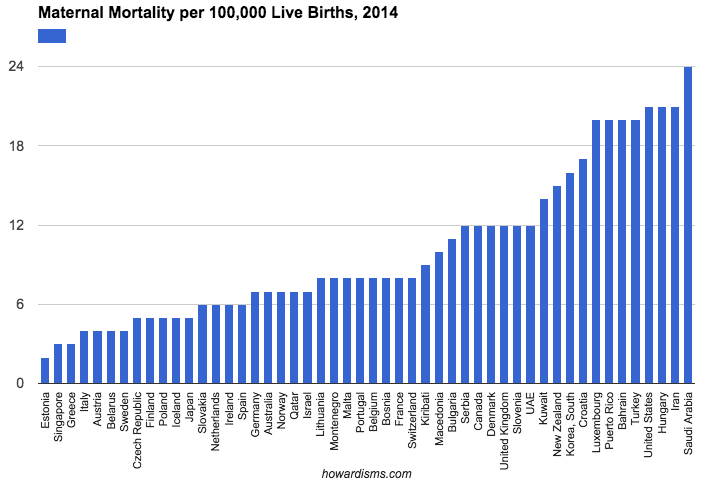
What should be noticeable immediately is that the countries with the lowest Cesarean rates also have the lowest rates of maternal mortality. The inverse is also true. So we definitely aren’t killing mothers by doing fewer Cesareans. How about babies though?
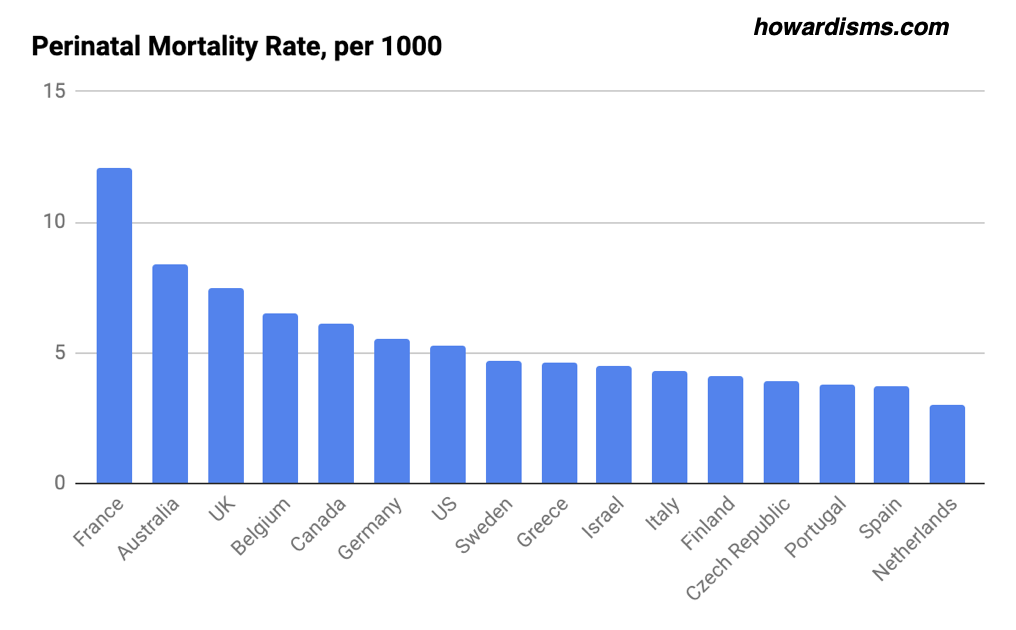
Let’s highlight some countries in the last three charts. The Netherlands has a very low perinatal mortality rate, a low maternal mortality rate, and a low Cesarean delivery rate. The same is true for Finland, Israel, and Sweden. A lot of the variation in perinatal mortality from country to country, at least of those listed, is related to the way the data is collected. You can’t get too excited about nation-to-nation comparisons. Still, it is clear that one can have a low Cesarean rate along with low maternal and perinatal mortality rates.
What about countries with even lower rates of Cesarean?
There are plenty of countries in the world with very low Cesarean delivery rates. In fact, there are at least 29 nations with a Cesarean delivery rate under 5%. But how do they compare in terms of outcomes? The chart below shows those countries listed in order of increasing Cesarean delivery rate along with their rates of maternal mortality and infant mortality. I had to use infant mortality rather than perinatal mortality because those data just aren’t available. Of course, the high rates of maternal and infant mortality are again related to dozens of other factors besides just the rate of Cesarean delivery but it shows the general trend that a low rate of Cesarean delivery is not a good indicator of maternal and child health.

By comparison, the rate of maternal mortality in Finland, which has a 15.8% Cesarean delivery rate, is 5 per 100,000 (compared to an average of 584 for the countries above) while the infant mortality rate in Finland is 17 per 10,000 (compared to an average of 610 for these countries). Yes, yes, yes … I know there are many more things that account for these differences, but my only point is that a big part of improving maternal and perinatal mortality is the introduction of a higher rate of safe Cesarean delivery.
A better comparison might be India, which has a Cesarean delivery rate of 9%. India is the most developed country in the world with a Cesarean rate under 10%. The maternal mortality rate in India, though, is still 122 per 10,000 (compared to 5 in Finland) and the perinatal mortality rate in India is 26 per 1000 (compared to 4.1 in Finland). Though many things account for these differences, it is fair to assume that a slightly higher Cesarean rate would naturally occur in India as part of improving these rates.
What about the United States?
At some point in US history, we have had a healthcare and maternity care system equal to all the systems currently present in the developing world. We had rates of maternal and infant mortality that were similar to all of the countries we have just discussed at some point in our history. So we might be able to learn something from our own development about where the appropriate rate of Cesarean delivery should be.
At the start of the 1970s, the Cesarean delivery rate in the United States was only 5.5%. Since then, it has grown to as high as 32.9% and hovers around 32% today. The following graph shows the rates of Cesarean delivery as well as the rates of maternal and perinatal mortality since 1970 along with some other major innovations that have influenced those rates apart from Cesarean delivery.

At the start of the 1970s, with a Cesarean rate of only 5.5%, we had a perinatal mortality rate of 28.9 per 1000, which is about what India’s is today. Our perinatal mortality rate today is just under 10. Our maternal mortality rate was 21.5 per 100,000 in 1970 and this number continued to decline to a low of 7.2 in 1987. After 1987, however, it has continued to increase to 17.4 – and the rising rate of Cesarean undoubtedly has largely contributed to this.
And for what benefit? The decline of our perinatal mortality rate from 14 per 1000 in 1987 to 9.64 in 2017 was almost certainly not related to an increase in the rate of Cesarean delivery. Instead, this is almost exclusively due to improvements in NICU care and survival rates of premature infants.
So, essentially, we have made no significant obstetric improvements since at least 1987. The truth is the actual year of decline likely comes a few years before since the effects on maternal mortality in particular lag a few years (since there is a higher complication rate among women with multiple Cesareans). That is not to say that we haven’t gotten better at providing critical care to pregnant women. We have. We have improved ICU care, availability of blood transfusion, protocols for management of obstetric emergencies, etc. But despite the reality that we have gotten much better at handling obstetric emergencies, women are still dying at a higher rate. Without all of these improvements, we very well might have a maternal mortality today in the US of over 30 per 100,000. This reality may push us closer to the year 1980 if we are to use this analysis to understand what the ideal Cesarean rate should be. In the US, the rate of Cesarean in 1980 was 16.5%.
One should resist making direct comparisons of US outcomes to other countries like Finland, including the Cesarean delivery rate. We collect data and label things differently and we have a significantly higher risk patient population than a country like Finland. Americans are heavier and less healthy in general. So I am more interested in trends than direct comparisons.
So what’s the answer?
My estimate is that the ideal Cesarean rate today should be between 15-19%. The upper figure is based partly on an important paper from 2015 that analyzed international data in a more formal way and partly from the data we have been discussing. If I were making the same estimate in 1980 I might have said that the ideal rate was between 10-15%. What’s the difference? The difference is simply the number of women alive today who have had previous Cesareans. I can control my own primary Cesarean delivery rate (which is around 6%) but I cannot control how many women come to me with previous Cesareans (sometimes several previous Cesareans). For a number of years now, I have performed more repeat Cesareans than primary Cesareans, despite having a very active VBAC practice.
In a world where there are fewer women with Cesareans (say, for example, the US in 1980 or Finland today), the range of estimates would be lower for this reason.
Why is it a range? Simply because the risk factors for patients vary widely by geography, hospital, and physician. Both lower Cesarean rates and higher Cesarean rates might be appropriate for given patient populations. But the average range, I believe, should today be between 15-19% with a goal of a decrement over time as fewer women with previous Cesareans are giving birth. This means that we absolutely must lower the primary Cesarean delivery rate to something under 10%. It is almost 24% in the US today.
But don’t midwives have a lower Cesarean rate than that?
No, not at all. There are two things to recall about midwife practices. The first is that there is a preselected population of low-risk women who are attended to by midwives. Most Cesarean deliveries occur in “high-risk” patients. These low-risk women are generally healthy women with few if any complications. In that population of women, the Cesarean rate should actually be between 2-6%. Where do I get this number? The lower number is an estimate appropriate for low-risk women with a prior vaginal delivery and the upper number is my own primary Cesarean rate, which is not risk-adjusted (most are for breech presentation). But about 15% of midwives end up transferring care of low-risk patients to the hospital or to obstetricians and the majority of those transferred receives a Cesarean delivery.
Well, geez, this is depressing. How can I do fewer Cesareans?
Glad you asked. Start with reading this post.
