Princess Charlotte of Wales
In the natural birth community, Pitocin is a dirty word. It is blamed, wrongfully, for nearly every ill that affects modern obstetrics: the high cesarean delivery rate, the pain associated with labor that leads women to want epidurals, postpartum hemorrhage, postpartum depression, fetal distress, autism, and just about anything else you can imagine. Some patients will do almost anything to avoid receiving some “Pit.” A quick Google search about oxytocin reveals countless horror stories and hysterical claims about the evils of this horrible medication that is a curse to modern women.
Pitocin, of course, is just a brand name for oxytocin. Oxytocin is made in the paraventricular nucleus of the hypothalamus and then released by the posterior pituitary. In 1954-1955, it became the first polypeptide hormone to be sequenced and synthesized. The American biochemist Vincent du Vigneaud won the Nobel Prize in Chemistry 1955 for his work on synthetic oxytocin. The commercial availability of synthetic oxytocin or Pitocin after the 1950s did radically change the practice of Obstetrics, but perhaps not in the way that many fear-mongers today claim.
To understand how it has changed Obstetrics, we first must understand what birth was like before so many interventions. Most patients who desire “a natural birth” long for the days before we started pumping dangerous chemicals into mamas and babies and interfering with and altering the natural process of childbirth. So here is a story to illustrate what birth was like before we screwed it up with so many interventions.
Charlotte, Princess of Wales
George III was King of Great Britain and Ireland, starting in 1760. At the time of his death in 1820, he was King of the United Kingdom and Ireland, as well as King of Hanover, which included territories that eventually became part of Germany.
George III was mentally unstable; “Mad King George” was thought to suffer from porphyria, and he had episodes of manic behavior and other irrational mood swings. The United States formed partly due to George’s madness. The US Declaration of Independence is essentially a list of his excesses. George was not liked very well in the United Kingdom either, particularly as his mental health deteriorated. His own subjects began looking to the future, when a new monarch would bring pride back to the throne and the United Kingdom, particularly after losing the American Revolutionary War. In fact, in the last ten years of his life, from 1810-1820, he was technically still king but his son, who would eventually succeed him as George IV, ran things due to George’s mental illness. But George IV wasn’t the future; his daughter was.
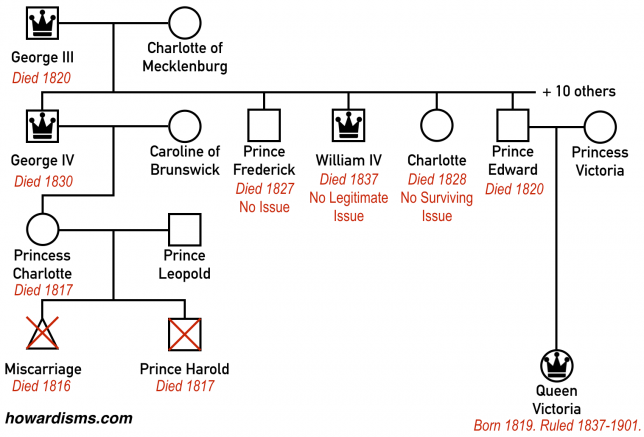
George IV’s only legitimate child was Princess Charlotte of Wales, born in 1796. She (or her children) were destined to inherit the throne. Since the monarch was both King of the United Kingdom and King of Hanover at the time, the people hoped that Charlotte would have a son, since Salic Law, which covered the Kingdom of Hanover, required a male to inherit. If a queen inherited, then the kingdoms would be split again. George IV wasn’t very popular either; he was a gluttonous, obese, alcoholic womanizer at his best. Like his father, he too lost a war to the US (the war of 1812). In the United Kingdom, public affections were directed towards the young Princess Charlotte, who was the only legitimate grandchild of George III at the time.
Charlotte eventually married a German prince called Leopold on May 2, 1816; Leopold would later become Leopold I, King of the Belgium. The two were widely celebrated and the young couple was adored by the public, in the same way that the marriage of Charles and Diana was celebrated in more recent times. The public hoped for a male heir to be produced by the union.
Charlotte quickly became pregnant and publicly acknowledged a miscarriage in 1816; some speculate she also had a second miscarriage. In July, 1817, it was announced that she was pregnant again and that she was expected to carry this pregnancy, due sometime in October of that year.
Charlotte had discussed with her friend, Lady Ashbrook, who should provide her prenatal care, and the women agreed upon Sir William Knighton. Unfortunately, the Queen made a different choice for Charlotte, and rather than Sir Knighton, a man called Sir Richard Croft was employed instead to attend to the Princess. Croft was known as the go-to obstetrician or accoucheur for the noble class, and decorum demanded that he be retained for the Princess rather than the perhaps more competent Knighton.
Croft’s care for her in the Fall consisted mostly of bed rest, dieting, and bleeding. Towards the end of the pregnancy, she had excessive weight gain and severe headaches, signs perhaps of “toxemia” or preeclampsia. These symptoms were met with more blood-letting to let out the toxins.
Her labor finally started with spontaneous rupture of membranes (SROM) at 42.1 weeks on Monday, November 3rd, 1817 at 7 pm. She was confined at Claremont House. Richard Croft was in attendance, and he called for back-up: his brother-in-law Matthew Baillie also was present. Baillie and Croft had married the twin daughters of Dr. Thomas Denman, a notable London Obstetrician who had written a textbook on the subject in 1788 and who had personally trained the two men.
Unfortunately for Charlotte, now post-dates and likely preeclamptic, she was not in labor when her water broke and initial progress was very slow. Her labor did start and she was noted to be complete at 9pm, November 4th, 26 hours after her membranes ruptured. Croft called for an operative obstetrician named John Sims, who arrived seven hours later (though he never examined the Princess). Some 15 hours after noting that she was completely dilated, the fluid turned to meconium-stained. Physicians of the time realized that this was an indicator of fetal distress.
Croft did not allow her to eat during her labor at all. A full 24 hours after becoming completely dilated – and 50 hours after her water initially broke – she finally delivered on November 5th at 9pm. A lifeless boy weighing 9 lbs (and who was later referred to as Harold because of Lord Byron’s poems) was born and futile attempts at resuscitation were made by Baillie and Sims in the adjoining room while Croft tended to the Princess.
The placenta was slow to separated and Croft performed manual extraction. She suffered a postpartum hemorrhage (PPH) and Croft left the placenta in the vagina to “tamponade” the bleeding. At about midnight, Princess Charlotte was suffering from nausea and vomiting and complained that she was hearing voices (delirium). She had chills and convulsions before becoming faint and quiet. She died at 2:30 am.
At post-mortem, she was discovered to have one pound of blood in her uterus. The infant appeared normal. They were buried together at Windsor Castle and a statue there shows Charlotte and Harold ascending into Heaven.
In the dust The Fair haired daughter of the Isle is laid,
The Love of millions, how we did entrust futurity to her.
– Lord Byron
The public was beside itself in mourning. The future of England had been lost. Many were quick to lay blame on Croft himself. A few months later, on February 13th, 1818, Croft was attending the birth of the wife of the Royal Chaplain, waiting in an adjoining room during a long labor much like Charlotte’s. Overcome with anxiety, he killed himself with a gun; next to his body was found a copy of Shakespeare’s Love’s Labor’s Lost turned to Act V, Scene II: “Fair Sir, God save you! Where is the Princess?”
Historians have called this the “triple obstetrical tragedy,” because the mother, infant, and obstetrician were all lost as a result.
George III was now left without a legitimate heir. Almost immediately, his surviving children who were able raced to produce a legitimate child. This almost three year period is British history is known as “the Baby Race.” Two of his sons abandoned their mistresses to take wives. Another bachelor quickly got married. The Duke of Clarence, the future King William IV, achieved a pregnancy first, but this was a premature child that died in 1819. This was followed by another 30 weeks loss. Prince Edward, the Duke of Kent, married Prince Leopold sister, Princess Victoria in 1818 and they had a girl in 1819 named Princess Alexandrina. George III died in 1820 and George IV became king until his death in 1830. William IV then reigned for 7 years until his death when finally Princess Alexandrine ascended to the throne at age 18, taking the name Queen Victoria in 1837.
Victoria married her first cousin and there are some other interesting Obstetric stories to be told regarding her, but this Queen, who would have never been born if not for the deaths of Charlotte and Harold, changed European history. She reigned for 63 years and had six children. When she ascended to the throne, because she was female, the Kingdom of Hanover was separated from the United Kingdom. The royal families became divided and competitive. There was a resurgence in German nationalism and continental resentment. Eventually, a large family feud broke out between her grandchildren, including George V, King of the United Kingdom, Kaiser Wilhelm of Germany, and her first cousin Czar Nicholas of Russia who had married her granddaughter. This family feud was called World War 1, and it killed more than 70 million people. The unresolved issues of World War 1 then led to World War 2, claiming another 85 million people.
Am I claiming that an obstetric accident in 1817 eventually led to the death of over 155 million people? Well, I guess I sort of am. Who knows how European history might have played out had Harold been born alive and eventually ascended to the throne. Perhaps the unification of the royal families of the United Kingdom and the Kingdom of Hanover would have stabilized central Europe or perhaps Queen Charlotte would have been a much different ruler than Victoria, not only handling European events differently but also treating India differently. We will never know. One thing is for sure though: if Charlotte (and Harold) hadn’t died that night, Victoria would have never existed and the people in power at the turn of the 20th Century would have never been born.
So let’s examine what went wrong with Charlotte’s pregnancy by performing a root cause analysis.
Charlotte’s death. The cause of death can be debated, but given what we know, it seems likely that shock secondary to hypotension, sepsis, or both was the culprit. The large amount of blood in her uterus discovered postmortem would seem to indicate uterine atony as a causative factor. She may have been anemic before labor started secondary to the antenatal blood-letting. Her rigors and chills, combined with 50 hours of ruptured membranes, makes infection also likely. When Croft decided to leave the placenta in her vagina as a “tamponade,” this likely just concealed the outlet for blood loss, causing it be unrecognized and retained in the uterus itself. The attendants actually left her alone shortly after delivery thinking all was well, clearly not recognizing that hemorrhage was continuing.
The practice of leaving the placenta in the vagina as a tamponade in cases of hemorrhage was unorthodox even for the time, but had been championed by Croft’s and Baillie’s father-in-law, Thomas Denman, in an 1816 edition of his textbook. More about Denman momentarily.
Today, we prevent women from becoming septic by responding to premature rupture of membranes with induction of labor, chiefly with Pitocin. Had Pitocin been available to Charlotte, she would have likely delivered almost 30 hours earlier and sepsis averted. If sepsis or chorioamnionitis had been present, today we treat with antibiotics. She very well may have been Group B Strep (GBS) positive, and today we would have screened her and treated prophylactically.
The resultant postpartum hemorrhage was no doubt precipitated by a tired and worn out uterus. The principle treatment (and prevention) for uterine atony is, once again, Pitocin. If we use birth in Africa as a means of comparison, it is reasonable to assume that Pitocin saves the lives of hundreds of women each week in the United States by preventing or treating postpartum hemorrhage (PPH) due to uterine atony.
If Charlotte did indeed develop preeclampsia before her labor started, as evidenced by the swelling and headaches that led to Croft’s bleeding treatments, then this too would have been solved in modern Obstetrics by timely induction of labor when signs and symptoms first started. This induction of labor would have likely been facilitated by – you guessed it – Pitocin.
Harold’s death. We can’t know the exact cause of Harold’s death, but we do know that he passed meconium (and was therefore still alive and in distress) at least 9 hours before he was born. Worse, by the time he passed meconium, Charlotte had been completely dilated for 15 hours but remained undelivered. The passage of meconium was recognized at the time as a sign of fetal distress; still, even though Charlotte was completely dilated, nothing was done for a full 24 hours of complete dilation and 9 hours after the observation of meconium.
What could have been done at the time? Forceps. The Chamberlen family had been using forceps to deliver babies (albeit in secret) since at least 1634. The family secret found its way into a textbook of Obstetrics by 1735 and at the time that Charlotte was laboring, forceps were widely used in Obstetrical practice. In fact, few providers would have hesitated to use forceps in this delivery, given the circumstances. However, one textbooks of obstetrics went against the grain and recommended a strict conservatism in the use of forceps, including the criteria that the fetal head had to be crowning for six hours before they were applied. Can you imagine crowning for six hours? You guessed it: that controversial criterion was in Thomas Denman’s textbook, the father-in-law of Croft and Baillie. It is quite reasonable to assume that nearly any other Obstetrician of the day would have intervened sooner, perhaps making a difference. Recall that Sims, who was proficient with forceps, had been called to the delivery and was present for 17 hours before Harold was finally stillborn. But Croft, who wanted all the glory of delivering the future monarch to himself, never allowed Sims to even examine Charlotte.
Even without forceps, one would think that Pitocin might have made for more effective contractions, delivering the child much sooner. If Harold died of sepsis, then we can also safely assume that things might have been different if Pitocin was used at the first, after her water broke. Perhaps he was already dead, due to post-datism? Or would have succumbed to meconium-aspiration syndrome? Perhaps there had been a prolonged abruption? Today, we would have induced Charlotte 8 days before her water broke, at 41 weeks, specifically to prevent these tragic outcomes (and we would have used Pitocin).
Croft was a diffident rule-follower, who lacked ingenuity, creativity, vision, or the ability to think for himself. His biographers have described him as average and just not that smart. Louis Hellman said of him,
A lonely man in the delivery room upon which the eyes of the world were focused, he had neither the fortitude nor the imagination to defy established tenets.
The blood-letting, the placenta-tamponade, the nonuse of forceps, the lack of deference to Sims – all of these things no doubt contributed to the triple tragedy (and perhaps the quadruple tragedy if you buy the World Wars hypothesis). The worst part is that Charlotte herself never wanted Croft as her Obstetrician; recall, she wanted Sir William Knighton. Might he have avoided Croft’s mistakes? We can’t know for sure, but we do know that his father-in-law was not Thomas Denman.
So the root cause is picking the wrong Obstetrician. But think of how different the world might be had Pitocin existed at the time and Charlotte had had an Obstetrician willing to intervene when the circumstances dictated it instead of being a coward.
Since the time of Charlotte and Harold’s death, maternal and neonatal mortality has dropped more than 100-fold. Pitocin is a big reason for this. Just like forceps, it should only be applied when needed; but when needed, it is life-saving.