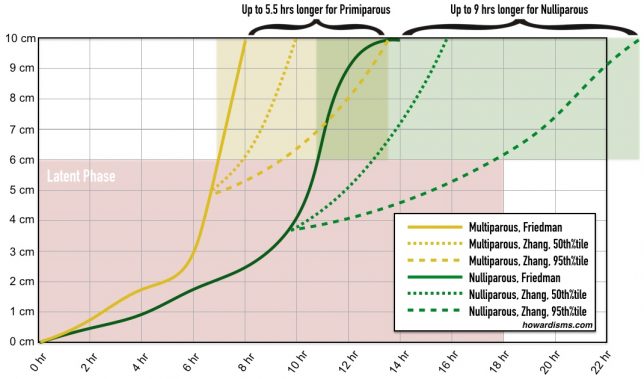
Comparison of Friedman and Zhang labor curves
I’ve noticed that a lot of doctors don’t like the suggestion that their cesarean delivery rate is too high. On one hand, many Obstetricians will admit that a primary cesarean delivery rate of 24% seems ridiculous; that it seems absurd that 1 in 3 women should have their babies cut out of their bellies. But, on the other hand, they aren’t quite sure how to make their cesarean delivery rates any lower. It seems like they’re following the rules but still ending up with too many cesareans. So let’s look at some practical strategies based upon the Obstetric Care Consensus series bulletin entitled Safe Prevention of the Primary Cesarean Delivery.
This bulletin, published in 2014, really did transform a lot of our practices. I remember when it came out. I literally stayed up half the night reading it, elated that ACOG and SMFM were finally taking a stand against the outrageous epidemic of unnecessary cesareans (unnecesareans). However, almost four years later, I suspect that not many people have made the transformative adjustments necessary to really see their patients benefit from this new guideline. So let’s look at the recommendations in detail and see how we may need to improve our practice patterns.
Let’s take a look at each specific recommendation:
- A prolonged latent phase (e.g., greater than 20 hours in nulliparous women and greater than 14 hours in multiparous women) should not be an indication for cesarean delivery.
Prior to this recommendation, it was not unusual to see a diagnosis of prolonged latent phase abused liberally as an indication for cesarean. First of all, the diagnosis of a prolonged latent phase of labor should theoretically only be made in patients who present in spontaneous labor, not inductions of labor. Because the latent phase extends from the beginning of labor until the point that the patient is in active labor, then the exact length of the latent phase can only be accurately determined retrospectively. Secondly, the definition of when active labor begins changed with the guideline from around 4 cm to around 6 cm dilation for most women. So, this new recommendation doesn’t suggest a replacement criteria, it simply says do not use a prolonged latent phase of whatever length as an excuse to do a cesarean delivery. The truth is, most diagnoses of a prolonged latent phase are inaccurate. Because the patient never reached the active phase of labor, it is ambiguous as to whether she was ever truly in latent labor. Therefore, this old indication for cesarean delivery lacks any objective validity. It should not be used.
- Slow but progressive labor in the first stage of labor should not be an indication for cesarean delivery.
A protracted latent phase of labor is also not an indication for cesarean delivery. In a very simplistic and sophomoric view of latent labor, the latent phase starts at 0 centimeters and ends with the onset of the active phase, now defined as starting at 6 cm. But think about it: there are patients who present at 41-weeks for induction of labor who are already 4 cm dilated; when were they 0 cm? Has their latent labor lasted for weeks? Of course not. Because the diagnosis of latent labor is necessarily retrospective and defined by when active labor started, then arrest disorders affecting latent labor should never be used as an indication for cesarean delivery. Again, no replacement criteria is offered. Slow change from 1 cm to 2 cm and from 2 to 3 cm, etc., may last hours to days to weeks.
- Cervical dilation of 6 cm should be considered the threshold for the active phase of most women in labor. Thus, before 6 cm of dilation is achieved, standards of active phase progress should not be applied.
The Friedman Curve and the average parameters of labor for nulliparous and multiparous women that medical students and residents have been made to memorize for decades have done more to promote unnecessary cesareans than almost anything else except for electronic fetal monitoring. The Friedman Curve was just wrong. It might have applied to the population of women that Friedman observed who presented in true spontaneous labor in the 1950s, but it doesn’t apply to women today. The curve and all of its derivative data and guidelines should be abandoned and medical students and residents need to stop memorizing the nonsensical parameters that have been drilled into their heads for 50 years.
In Friedman’s data, 4 cm seemed to be the average inflection point on the labor curve where active labor started. But 6 cm is the point observed in modern-day data sets (Zhang, et al.). 6 cm is not an absolute rule for every patient since, once again, you can only know for sure when active labor starts by looking retrospectively at the rate of cervical change over time. But the point of the 6 cm guideline is that all of the labor dystocia guidelines applied to the active labor phase should not be used in women who are not at least 6 cm. That means that you can’t use the arrest of dilation rules in a woman who is only 5 cm. This one change in the guidelines, if followed appropriately, will make more of a difference in reduction of the cesarean delivery rate than almost any thing else.
Look at the illustration at the beginning of this post. You can see the differences in the average labors recorded in Friedman’s data compared to Zhang’s data. But even more telling are the curves for Zhang’s 95th percentile data; we really shouldn’t begin to define something as abnormal in until it has fallen beyond the 95th percentile. If anything, it’s these 95th percentile graphs that we should memorize so that we can identify those labors that are abnormal. Even at that point it doesn’t mean that a cesarean delivery should occur, but it does mean that interventions like augmentation are needed. Notice that primiparous mothers may have labors that last up to 5.5 hours longer than Friedman’s data would suggest while nulliparous mothers may need up to 9 hours longer; and that’s just in the active phase, let alone the latent phase. Erase the Friedman curve from your mind. Abandoning the curve cuts the cesarean rate in half.
- Cesarean delivery for active phase arrest in the first stage of labor should be reserved for women at or beyond 6 cm of dilation with ruptured membranes who fail to progress despite 4 hours of adequate uterine activity, or at least 6 hours of oxytocin administration with inadequate uterine activity and no cervical change.
The old so-called “2 hour rule” is deeply ingrained in the hearts and minds of Obstetricians. It gets them home quicker, and is a popular excuse for unnecessary cesareans. So-called “failure to progress” or “cephalopelvic disproportion” are widely misused diagnoses used to justify cesarean deliveries. But this guideline should mostly eliminate those types of cesarean. Two of the three principles of this diagnosis have changed.
The first is that 6 cm rather than 4 cm is used to define the boundary of active labor that we’ve already discussed.
The next is that there must be no documented cervical change for at least 4 hours, not just 2 hours. Think about this: under the old criteria if a woman were 4 cm for 2 hours, you could do a cesarean delivery. But under the new guidelines, she would have to be 6 or 7 cm with no change at all for 4 hours in order to do a cesarean delivery.
In both cases, she is also required to have adequate uterine activity. Residents and medical students used to memorize that 3 contractions in 10 minutes was adequate uterine activity. But the current minimum uterine activity required to be considered adequate is it least 200 Montevideo units (MVUs), which would usually corresponds to about 4.5 strong contractions in 10 minutes. Though the guideline doesn’t explicitly say this, we know from original research defining Montevideo units that about 40% of women in spontaneous labor have MVUs greater than 300. So the other lesson is don’t stop once you get to 200 MVUs. Unfortunately, when 200 MVUs was defined as adequate a lot of labor units created oxytocin protocols designed to get patients to this threshold and then stop. But there is no science behind this. 200 was a minimum, not a maximum, and we know that about 10-20% of women will fail to progress with only 200 MVUs. If you stop increasing the oxytocin just because you have achieved 200 MVUs, you are accepting the fact that 10-20% of your patients will have arrest disorders due to inadequate uterine activity even though 200 MVUs were achieved. The criteria for not increasing oxytocin further should be tachysystole or five or more contractions in 10 minutes.
- A specific absolute maximum length of time spent in the second stage of labor beyond which all women should undergo operative delivery has not been identified.
This guideline, like the latent phase guidelines, does not suggest a replacement standard. It does state that there is no evidence of harm with a longer length of the second stage of labor. The truth is, even under the old guidelines, most women were not given an adequate length of time in the second stage. Obstetricians don’t like pushing. They aren’t good at it. If docs feel like things aren’t going where they should after an hour or so, cesareans are handed out like water. This has been all the more true if the Obstetrician was biased by something like the presence of gestational diabetes or something else that may them a bit timid. But these are mostly emotional responses.
Today, it’s unusual for an obstetric resident to see a patient have success after 2 or 3 hours of pushing. They aren’t allowed to see it that often. But the guideline allows patients to have at least these lengths of time to push. Between dense epidurals and poor pushing technique, there are lots of reasons why some women might need a longer time to push. The fetal head needs to mold, and even when progress doesn’t seem apparent, progress is being made. Nurses and doctors want to shorten the second stage because of old fables like cervical swelling or excess molding of the head. These are not scientific indications for second stage problems but are anecdotal observations that are used as an excuse to predict failure even when failure doesn’t exist. Obstetricians are also not very good at correcting asynclitic heads and rotating persistent occiput posterior babies. Efforts with either of these could tremendously shorten the second stage for many women.
- Before diagnosing arrest of labor in the second stage, if the maternal and fetal conditions permit, allow for the following:
- At least 2 hours of pushing in multiparous women (1B)
- At least 3 hours of pushing in nulliparous women (1B)
- Longer durations may be appropriate on an individualized basis (e.g., with the use of epidural analgesia or with fetal malposition) as long as progress is being documented.
Again, notice the difference in the guideline. The classic rule that every medical student has memorized is that multiparous women get one hour and nulliparous women get two hours with an additional hour added if she has an epidural. This is no longer the rule. Multiparous women, even without an epidural, get at least two hours of pushing time and nulliparous women without an epidural get at least three hours of pushing time. Then you may choose to extend the pushing time even further if the patients have an epidural or other factors that might have contributed to the length of their second stage of labor, like fatigue, resting periods, or poor effort. These new second-stage guidelines require a significant culture change. Even under the old guidelines, as I stated above, Obstetricians would rarely give women longer than about an hour to push. Many could not imagine giving an nulliparous woman with an epidural 4 hours or longer to push.
- Operative vaginal delivery in the second stage of labor by experienced and well trained physicians should be considered a safe, acceptable alternative to cesarean delivery. Training in, and ongoing maintenance of, practical skills related to operative vaginal delivery should be encouraged.
The cesarean delivery has become the forceps of modern Obstetricians. A surprising number of currently practicing Obstetricians do not use either vacuums or forceps as part of their obstetric practice; even among those who still do, most are reticent to use them after a patient has had prolonged pushing during the second stage for fear of failure or pulling themselves into a shoulder dystocia. The guideline is reinforcing the safety and efficacy of operative vaginal delivery with this recommendation.
- Manual rotation of the fetal occiput in the setting of fetal malposition in the second stage of labor is a reasonable intervention to consider before moving to operative vaginal delivery or cesarean delivery. In order to safely prevent cesarean deliveries in the setting of malposition, it is important to assess the fetal position in the second stage of labor, particularly in the setting of abnormal fetal descent.
Like operative vaginal deliveries, this skill too is lacking amongst most modern Obstetricians. Unless residents are trained and taught to embrace the practice of manual rotation, it will certainly never happen in their own independent practices. We should be more skilled at manual rotation than the generations that have come before us because we can use bedside ultrasound to accurately assess the fetal position and our progress at manual rotation. But, unfortunately, the skill is not being taught. Physicians are commonly not even assessing the position and rotation of the head during labor as they allow nursing staff to perform all the cervical exams and push with the patient for some length of time before coming over at 5 PM from the office and doing a cesarean because it’s been 3 hours of pushing already with a malrotated head. Nurses can be trained to assess the position and rotation of the fetal head, but it is the responsibility of the physician to assess these factors. The guideline reinforces the efficacy and importance of manual rotation.
- Amnioinfusion for repetitive variable fetal heart rate decelerations may safely reduce the rate of cesarean delivery.
It’s true that amnioinfusion likely doesn’t do much, if anything at all, to make fetal outcomes better, but it has been shown to reduce the risk of cesarean delivery. Most patterns of repetitive variable decelerations can be markedly improved with an amnioinfusion and then the anxiety of the nursing staff and physicians can be improved. If a cesarean delivery is being considered for repetitive variable decelerations without an amnioinfusion having already been performed, then one of the strongest and most evidence-based recommendations in this guideline is being violated.
- Scalp stimulation can be used as a means of assessing fetal acid–base status when abnormal or indeterminate (formerly, nonreassuring) fetal heart patterns (e.g., minimal variability) are present and is a safe alternative to cesarean delivery in this setting.
This is the only other specific recommendation about fetal monitoring that the guideline makes. That doesn’t mean that there aren’t many other things that we can do to decrease the risk of unnecessary cesarean delivery for perceived abnormalities of fetal heart tracing. Scalp stimulation which produces a fetal acceleration is a very reassuring finding and can be used to predict normal fetal acid-base status in patients with absent or minimal variability. This is especially important in a day and age where many fetal tracings are relatively flat due to maternal opioid abuse. Units should also implement specific protocols for fetal tracing management as I suggest here.
- Before 41 0/7 weeks of gestation, induction of labor generally should be performed based on maternal and fetal medical indications. Inductions at 41 0/7 weeks of gestation and beyond should be performed to reduce the risk of cesarean delivery and the risk of perinatal morbidity and mortality.
This recommendation about avoiding unnecessary induction of labor before 41 weeks has probably created more angst and controversy than almost any other recommendation in the guideline. If you follow the literature that’s been published subsequent to the arrival of this guideline, you’ll notice a cadre of Obstetricians who are angry at many of the recommendations because they don’t comport with what they’ve done their entire careers. The ARRIVE Trial and similar studies have been conducted to attempt to prove that induction at 39-weeks of nulliparous patients is not associated with a higher risk of cesarean delivery. But, as I pointed out here, that’s only true if your baseline expectation of a primary cesarean delivery rate is over 20%.
The high-quality evidence that this recommendation is based upon comes from data from several years ago when the primary cesarean delivery rate for low-risk nulliparous women was nowhere near 20%. Yes, this recommendation only applies to low-risk nulliparous women with unfavorable cervices, not those with high-risk indications warranting delivery before 41-weeks or other automatic indications for cesarean delivery like placenta previa or malpresentation. This recommendation really is at the core of the problem. If you believe that it is acceptable to perform a cesarean on nearly 1 in 4 low-risk healthy women at term, then there’s probably little to do to change your mind. But don’t act like you’re practicing evidence-based medicine.
- Cervical ripening methods should be used when labor is induced in women with an unfavorable cervix.
This seems obvious to state, but the rule is violated all the time. Uncertainty exists about what the definition of “unfavorable” is and some uncertainty still exist about what the best method for cervical ripening might be. But since this guideline was published, new high-quality research makes one thing clear: the best method of cervical ripening is use of a single balloon Foley catheter placed intracervically accompanied by either misoprostol or oxytocin. The guideline throughout assumes that you’re giving things your best effort. When it says that you should give the patient oxytocin for some amount of time, it assumes that you are using oxytocin in a reasonable way and not just leaving it set on 2 mu/min for hours on end. Likewise, the guideline assumes that you’re going to use the best available methods for induction and ripening of the cervix. So, the days of “low-dose” oxytocin, cervidil, and other ineffective modalities of ripening and augmentation should be abandoned. By the way, nipple stimulation, breast pumping, intercourse, and Mexican food don’t count as attempts at cervical ripening either.
- If the maternal and fetal status allow, cesarean deliveries for failed induction of labor in the latent phase can be avoided by allowing longer durations of the latent phase (up to 24 hours or longer) and requiring that oxytocin be administered for at least 12–18 hours after membrane rupture before deeming the induction a failure.
This recommendation may seem confusing at first. Pay attention to what it does say and not what it doesn’t say. It says that an induction of labor can be allowed to take up to 24 hours or longer. Thirty-six hours is longer than 24 hours and is therefore within the scope of the recommendation. Twenty-four hours is not a line in the sand; it is a minimum. Much like 200 Montevideo units was a minimum that became a maximum in the eyes of many, so too is 24 hours being interpreted as a maximum length of the latent phase. But, recall, we eliminated all the latent phase of labor recommendations because the latent phase of labor is a subjectively defined interval. If we are not going to use latent labor boundaries in women who are in spontaneous labor, we certainly cannot use them in women who are undergoing induction of labor.
So, the latent phase should be allowed to last at least 24 hours or longer. Within that time period, however long it might be, the patient should have ruptured membranes for 12 to 18 hours with concurrent use of oxytocin. You don’t get credit for following the guideline if you rupture membranes at 1 cm and start oxytocin and then perform a cesarean 12 hours later. Again, the guideline assumes that you are giving this your best effort. Thus, you should likely avoid rupture of membranes until there has been adequate cervical ripening, meaning when the patient is 3 or 4 cm dilated. Also keep in mind that the recommendation is about the length of time to get the patient to the active phase, not to delivery.
Failed inductions of labor should be quite rare. I would never do this to a patient, but the guideline allows for it: Imagine that a patient presents for induction of labor. Her cervix is closed and thick. She receives cervidil for 12 hours. Her cervix is unchanged. Then she receives four doses of misoprostol every 3 hours. Her cervix is now 2 cm dilated after 24 hours of cervical ripening. Four hours after the last dose of misoprostol, she is given oxytocin. Six hours after the start of oxytocin, she becomes 4 cm dilated. She then undergoes rupture of membranes. The pitocin is increased and 18 hours after rupture of membranes she is now 6 centimeters, dilated, and entering the active phase. All of this is still within the scope of the guideline, even though it took 52 hours to get her into active labor. There is no 24-hour rule.
As I said before, I would not torture a patient like this. A more reasonable method of induction would have been placement of a cervical Foley catheter along with concomitant use of oxytocin or misoprostol, followed by rupture of membranes after the Foley is expelled at around 4 cm and concurrent use of oxytocin. This strategy usually results in delivery within 24 hours.
- Fetal presentation should be assessed and documented beginning at 36 0/7 weeks of gestation to allow for external cephalic version to be offered.
About 3.8% of fetuses are not cephalic at term. If you are not actively checking for presentation and offering external cephalic version as a remedy to your patients, you will automatically have at least a 3.8% primary cesarean delivery right. Unfortunately, like assessment of intrapartum fetal rotation, many Obstetricians have not made it a part of their practice to routinely confirm cephalic presentation at term. If they do, it is only to schedule a cesarean delivery – not to offer external cephalic version. I even know of Obstetricians who go ahead and schedule the cesarean at 32 weeks if the baby is not cephalic. This, of course, is absurd. External cephalic version is also a dying art. Yet, it is effective almost two-thirds of the time and it is safe.
Many Obstetricians counsel their patients about external cephalic version but don’t do so in good faith. You and I both know that we can either talk a patient into it or talk a patient out of it depending upon how we counsel them. Again, the guideline assumes that you will present evidence-based and appropriate counseling to the patient, not try to make excuses for not doing it. The vast majority of women who have a noncephalic presentation at 36-37 weeks should undergo external cephalic version. The fact that the fluid is a little low or the placenta is a little anterior or the baby is a little big or the mom is a little hefty are all not contraindications to the procedure.
- Cesarean delivery to avoid potential birth trauma should be limited to estimated fetal weights of at least 5,000 g in women without diabetes and at least 4,500 g in women with diabetes. The prevalence of birth weight of 5,000 g or more is rare, and patients should be counseled that estimates of fetal weight, particularly late in gestation, are imprecise.
This recommendation could not be more explicit. If you are counseling patients with babies below these weight thresholds that they should undergo cesarean delivery electively for a large baby, you are just on the wrong side of science. The evidence is clear that offering cesareans for weight thresholds below these parameters does not improve fetal outcomes. Yet, far too many cesareans are performed for purported macrosomia. The bulletin states that 4% of primary cesareans are performed for this indication. This would mean that roughly 1% of all women are delivered electively by cesarean for fetal macrosomia. Frankly, I am surprised that the number is this low. I suspect that some cesareans for macrosomia are hidden in other reported indications like “maternal request” or “maternal-fetal indications” or “other obstetric indications.” I know of practices that do a cesarean a week for big babies.
In any event, I can assure you that 1% of the babies born in your unit each year do not weigh over 11 lbs. The bulletin also states in the text that “ultrasonography for estimated fetal weight in the third trimester should be used sparingly and with clear indications.” Yet, many Obstetricians perform a early-term ultrasound routinely and women suffer as they undergo excessive numbers of cesarean deliveries for no reason. Remember that ultrasound has a very large margin of error (±20%) and unless there is sufficient pretest probability for suspicion of macrosomia (in other words, an indication like maternal diabetes or excessive maternal weight-gain), then you may be applying the excessive margin of error of ultrasound to a population at exceedingly low-risk, meaning that you will see mostly false positive results.
- Women should be counseled about the IOM maternal weight guidelines in an attempt to avoid excessive weight gain.
This recommendation doesn’t say that you should perform cesarean deliveries on women because they’ve had excessive maternal weight-gain, rather it states that you should try to prevent excessive maternal weight-gain as a means of reducing the risk of cesarean.
- Perinatal outcomes for twin gestations in which the first twin is in cephalic presentation are not improved by cesarean delivery. Thus, women with either cephalic/cephalic-presenting twins or cephalic/noncephalic presenting twins should be counseled to attempt vaginal delivery.
Over 1% of pregnant women carry twins. Around 90% of twin pairs have the first fetus presenting vertex. The guideline is very clear: women with a first twin who is cephalic-presenting should be counseled to have a vaginal delivery. Unfortunately, in spite of this clear-cut guideline and the evidence-based benefits to vaginal delivery for twin pregnancies, most Obstetricians in America consider a twin pregnancy an automatic cesarean delivery.
- Individuals, organizations, and governing bodies should work to ensure that research is conducted to provide a better knowledge base to guide decisions regarding cesarean delivery and to encourage policy changes that safely lower the rate of primary cesarean delivery.
This last recommendation is a catch-all. There are lots of other reasons why cesarean deliveries are performed. Many are not evidence-based. Women with certain cardiac or neurological abnormalities are routinely recommended to undergo cesarean delivery even though there is no medical reason for it. Women who develop certain complications like HELLP syndrome are often encouraged to undergo primary cesarean delivery even though they are still candidates for induction of labor. I saw a patient once who had a 600 ml blood loss with her first vaginal delivery so her Obstetrician told her she should have a cesarean next time (with an average blood loss of 1 L) because of her history of hemorrhage. There is much room to improve all our recommendations for which patients might benefit from cesarean delivery and which patients do not, but these recommendation should be based upon rigorous evidence, not anecdotal opinion.
It seems like today almost any reason will suffice to justify a cesarean delivery. But let’s remember the purpose of these recommendations: A woman undergoing a cesarean delivery is nearly four times as likely to die as a woman undergoing a vaginal delivery; she is nearly five times as likely to suffer from an amniotic fluid embolism; she is three times as likely to have a severe complication. Each subsequent pregnancy will become more dangerous for her. And, no, she is not less likely to have urinary incontinence because she avoided that horrible vaginal delivery. Cesarean delivery is not a panacea for all matters obstetric; it is a life-saving tool that should be used only when needed. Like all of the best inventions of modernity, it is both good and bad.
Let’s review briefly some typical indications for cesarean:
- Failure to progress: this term is no longer used.
- Labor dystocia: this term is no longer used.
- First stage arrest: can be justified when 1) the cervix is at least 6 cm dilated AND 2) there has been no cervical change for at least four hours AND 3) there are adequate uterine contractions. If adequate contractions cannot be achieved, then the duration should be at least 6 hours.
- Second stage arrest: can be justified if no delivery with three hours of pushing in a nulliparous patients and two hours with a multiparous patient; add more time (perhaps an hour) if the patient has an epidural.
- Failed induction: can be justified if at least 24 hours has been dedicated to achieving active labor with at least 12-18 hours of oxytocin with ruptured membranes.
For more information, read this.