(Hit play if it doesn’t play automatically. Video from here.)
There are a variety of reasons why some parents may choose to not vaccinate their children; most are unscientific and have their origins in fear-mongering. I never get too worked up about patients who oppose vaccinations. The crippling self-righteousness of some physicians who are confronted with an anti-vaxxer parent is non-productive and in many cases exceedingly hypocritical. I am more concerned about a physician who rejects evidence-based medicine, even though they have been trained appropriately, than I am concerned about a parent who has been made scared about vaccine safety by sensationalistic media (Robert DeNiro, Jenny McCarthy, Ellen Degeneres, Dr. Oz, etc.) The concerned parent, at least, has no training in the subject matter. While just a small percentage of parents oppose vaccines, most physicians practice non-evidence-based medicine; so the adage rings true: Physician, heal thyself.
In any event, many thoughtful parents are genuinely conflicted by the potential ethical issues that arise with giving their children vaccinations. These ethical issues can be summarized in the following manner:
- Is it ethical to give a child, who cannot consent, a potentially dangerous vaccine?
- What is the ethical burden, to the parent, of giving the child a vaccine that might cause more harm than it might prevent?
I would also add the following ethical concern from a societal perspective:
- Is it ethical for someone to benefit from herd immunity present in the community without taking any risk (or having any buy-in)?
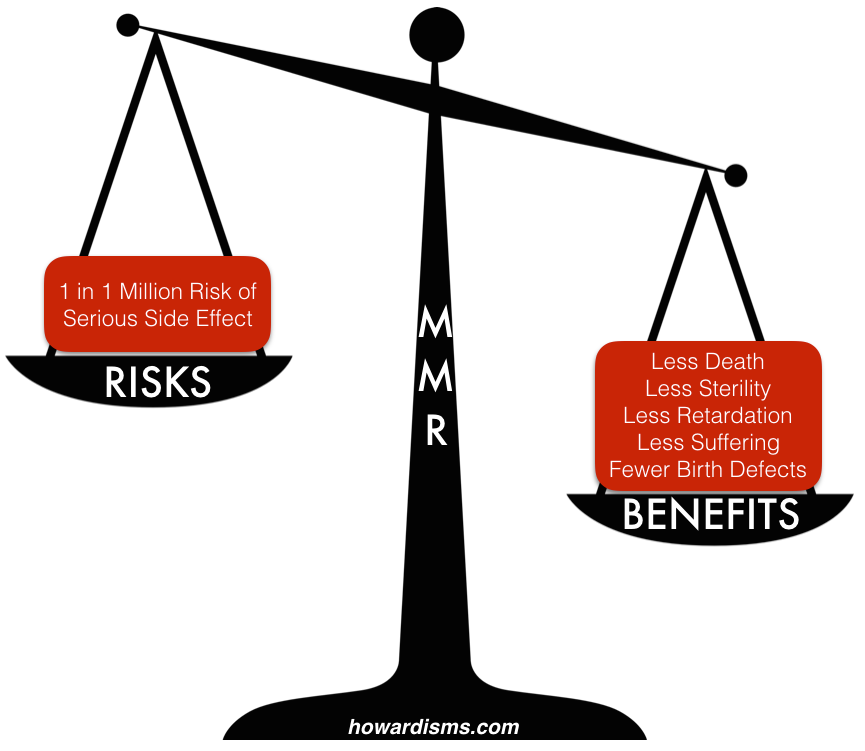
These ethical questions must be answered regardless of how harmful or how effective vaccinations truly are; in other words, these concerns don’t magically melt away just because a physician (or all of science) declares that vaccines don’t cause autism or some other claimed problem. The fact is, vaccines do have some degree of measurable risk and some degree of measurable benefit. I gave an example of this in From One Extreme to the Other… which I will briefly summarize again regarding the MMR vaccine.
What are the risks of the MMR vaccine? 1 in 6 children get a fever; 1 in 20 get a mild rash; 1 in 75 get swelling in the lymph nodes; 1 in 3,000 have a seizure related to fever; 1 in 30,000 develop transient thrombocytopenia; 1 in 1 million develop a serious allergic reaction, with even fewer reporting deafness, coma, or brain damage.
What are the benefits of the MMR vaccine? The virtual elimination of measles, mumps, and rubella. From 1963-1983, it is estimated that the vaccine prevented 52 million cases of measles in the US, along with preventing 17,400 cases of intellectual disability, and 5,200 deaths. Prior to the introduction of the mumps vaccine, there were about 150,000 cases each year, many leading to sterilization of young boys; since the introduction of the vaccine, only about 265 cases are reported each year (mostly in unvaccinated children). Prior to the vaccine, rubella caused countless cases of congenital rubella syndrome in pregnant women; over a 100,000 cases still occur worldwide in unvaccinated areas of the world, but the condition has been eliminated in the US.
We make decisions for ourselves and our patients by weighing the risks and benefits; in this case, the benefits of the MMR vaccine far outweigh the risks. Still, the ethical questions remain, particularly in the case of a young child who cannot make informed decisions for herself.
In other words, parents are aware that some risk of death awaits the child who gets a vaccination. We believe that this risk is less than 1 in 1 million (the mother may wrongly believe that it is higher), but when she takes that chance (whatever the chance is) to reduce her risk of getting some disease (whatever that risk is), she is making the decision to do something potentially dangerous (no matter how small the risk) to get some unknown payoff. The payoff is unknown because the mother cannot know exactly what her child’s risk of measles, mumps, and rubella actually is, and this makes the decision more difficult because, in her mind, the benefits are unknown while the risks are more concrete.
Regardless, all that is important is that we believe that the benefits outweigh the risks. If they do, then the patient who takes a vaccination makes a good decision and the mother who gives the child a vaccine makes a moral and ethical decision. In fact, it would be unethical to not give the vaccine (if the benefit actually is greater than the risk). To understand this, we must first really appreciate that every human activity has risk; there are no “safe” interventions. When we drive an ambulance to the hospital, there is a risk of death; when we give a child food to eat, there is a risk of death; when we walk in the rain, there is a risk of death. In each situation, we choose to take some (small) risk because the benefit is greater.
Nearly 1,000 children die in car crashes each year. We seek to minimize that risk (car seats, speed limits, safe cars, DUI-enforcement checkpoints, etc.), but it still happens. By contrast, about 100 children die each year from vaccines. A reasonable parent might make a decision not to strap her child into a vehicle designed to travel down the highway at 70 mph amid other such vehicles, often in the control of less than perfect drivers; but when she does drive her child somewhere, it is because the benefit of that trip is felt to be greater than the risk of that individual trip. So, too, the parent must feel in respect to vaccination.
Conversely, if an ambulance didn’t take someone dying of a heart attack to the hospital or if a parent didn’t provide food to a child, the consequences are clear. Choices like these are seldom questioned because the consequence of non-action is so clear, but both actions still carry potentially fatal risks. With vaccines, the consequences of non-action are less clear to patients, so we must do a better job of communicating those real risks.
Nevertheless, whenever the benefit of vaccination is greater than the risk, the vaccine should ethically be given, and this is true for all things in life. The fact the child doesn’t participate in the decision is irrelevant; the child doesn’t participate in the decision to be fed or kept warm either, but we choose these potentially dangerous interventions (picture food poisoning and house fires) because the benefits outweighs the risks.
Parents also worry about forgiving themselves if the dreaded complication of vaccination should happen to their child, like death. But this worry only occurs because the parent has a difficult time internalizing that the chance of a bad outcome is greater for their child if they do not get the vaccine. When this belief is internalized, the choice is obvious, unequivocal, and inherently ethical. How could they forgive themselves if the child died or became handicapped by a disease for which a vaccine was available?
Discussions with parents should focus on this type of value proposition: “If your child is vaccinated, there is less than a 1 in 1,000,000 chance that a severe complication will occur including death – the risk of being killed by lighting is 1 in 200,000; on the other hand, if your child is not vaccinated, there is about an 8 in 1,000,000 chance that your child will die a preventable death. Other minor and self-limited reactions may occur with vaccinations but for each minor reaction dozens of children will not get a potentially severe illness that could lead to death or disability.”
The numbers I listed above are the current statistics, not the historical statistics. The individual patient who chooses not to vaccinate her child still largely benefits from heard immunity, as the graphic above illustrates. Even with herd immunity, the benefits still outweigh the risks – and it is important that parents understand this. The current rate of vaccination in the US is still around 90%, depending on the vaccine; the graphic above demonstrates that the benefits of vaccination would only increase as rates of vaccination, and therefore herd immunity, decrease. Large outbreaks are rare today due to herd immunity. Preventable diseases killed almost half of children by the age of 5 in the 19th century, but today we (vaccines) have made this unimaginable. In 2012, 15 infants died during an outbreak of whooping cough in the US, while about 60,000 people died worldwide from the disease; this shows how well herd immunity truly works.
This brings us to the last question: Is it ethical to benefit from herd immunity present in the community without taking any risk (or having any buy-in)? Many savvy parents are aware that cases of polio and other diseases that we vaccinate against are almost unheard of today, and they realize that, due to the rarity of these diseases and the fact that more than 90% of their neighbors have vaccinated their children, they can likely get away with not vaccinating their own kids, thus sparing their own children the 1 in a million chance of a bad outcome related to vaccines.
There are two problems with this idea, though.
The first I have already pointed out: even with herd immunity, parents are still better off vaccinating.
But the second reason is the ethical one: Herd immunity is something that society does to benefit society. It works best when we all do it, though there are some who can’t, like immune-compromised children or kids with specific allergies. There are also children who are just non-responders. This segment of the population still doesn’t usually get polio because the rest of us chip in and get our vaccinations, and presumably they would too if they could.
But the folks who can vaccinate but choose not to are stealing from the rest of us. We buy car insurance to distribute risk, and we don’t pay out when someone wrecks his car unless he has previously paid into the pool. Why? Because this is the ethical and moral thing to do. I can understand why a person would love to get all of the benefit while assuming none of the risk, but apart from the selfishness of this mentality, it practically fails because they are still at substantially higher risk than those who do vaccinate and those risks are growing geometrically as more patients opt-out. As you might imagine, unvaccinated children were disproportionately represented among the infections and deaths of the 2012 whooping cough outbreak, but vaccination rates were still about 75%. Imagine if vaccination rates dropped to 50% or lower? The graphic above can help you see the effect.
Patients think about vaccinations in the terms I have described. The more we are able to quantify risk and benefit to them, and not just negate their concerns as silly or unscientific, the more patients will listen to reason.