One of the obvious benefits of a laparoscopic surgical approach compared to an open approach is less pain and morbidity related to smaller incisions and less wound morbidity. Postoperative pain in general is reduced with laparoscopic surgeries, but a unique type of pain is found in up to 80% of surgeries: post-laparoscopic shoulder pain (PLSP), which is thought to be related to residual carbon dioxide causing diaphragmatic irritation of the phrenic nerve, as well as phrenic nerve neuropraxia. This type of pain doesn’t respond to pain medications as well as pain that is related to the incisions or the surgery itself does. Clearly, not all laparoscopic surgeries are created equal and levels of postoperative pain vary widely. Here are four tips to reduce postoperative pain related specifically to laparoscopic surgery.
1. Get the gas out.
Since there appears to be a relationship between the residual amount of gas and PLSP, then getting all the gas out would seem to be important. At a minimum, you should allow the capnoperitoneum to drain from an open, distal trocar (the lowest one) while applying gentle abdominal pressure. But better than that is to use the pulmonary recruitment maneuver (PRM). To do this, place the patient in 30° of Trendelenburg while opening the most distal trocars (this encourages the gas to rise to the lower abdomen); then have the anesthesia provider provide five manual pulmonary inflations up to 60 cm H20. Have the anesthetist hold the last inflation for five seconds. This maneuver increases the intra-abdominal pressure. Then flatten the patient and remove the trocar. This simple step has been shown to reduce PLSP-type pain from 64% to 31% and also reduce postoperative nausea or vomiting from 56.5% to 20.4%. It also reduced the need for postoperative pain medication. A recent study has shown that this maneuver works just as well even if the inflation pressure is only 40 cm H20.
2. Make smaller holes (but not necessarily fewer).
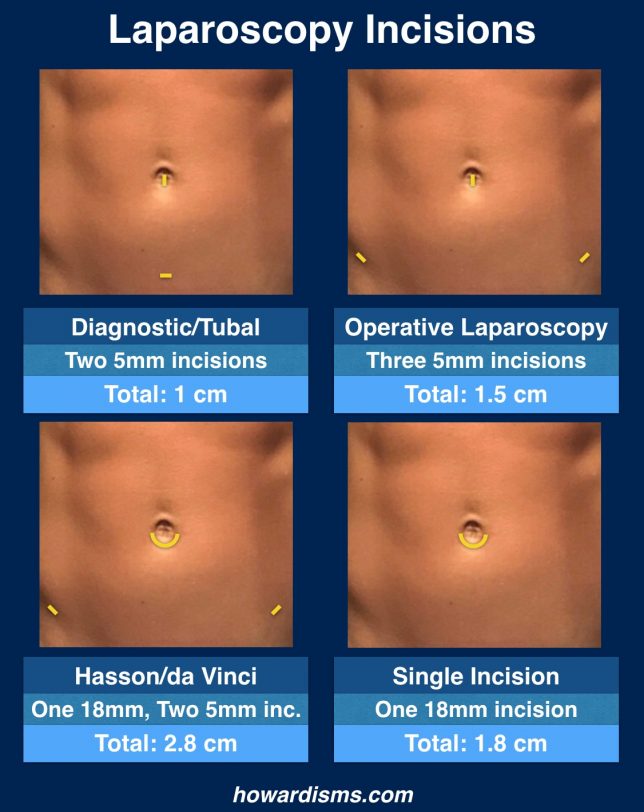
This sounds intuitive; one of the obvious advantages of doing a case endoscopically compared to doing it through a laparotomy is the smaller incisions. But remember, the smaller the better. If you can use a 5mm trocar, you’ll have less pain than if you use a 10 mm trocar. Modern instrumentation and optics has made larger trocars all but unnecessary. However, reducing the number of incisions by converting to single-port access laparoscopy doesn’t help reduce pain. Most gynecologic cases can be completed easily with two or three 5-mm trocars. Some diagnostic laparoscopies need only one 5 mm umbilical trocar. Almost all gynecologic surgeries can be performed through a single umbilical port as well, including hysterectomies, but that single port is usually about 18-mm. But don’t fall for the hype. Evidence shows that single-incision surgeries provide no advantage and take longer, but they don’t reduce pain and they are associated with higher risks of herniation through the larger umbilical incision.
Of course, if you are performing open laparoscopy with a Hasson cannula, you are probably already making a 15 to 18-mm hole and single incision surgery might provide an advantage. But you should be using a 5 mm direct entry trocar in the umbilicus and replacing this small incision with a larger incision is associated with more pain and hernianation risk.
By the way, if you perform sterilizations with a Filshie clip applicator, you don’t need an 8-mm or 10-mm port to insert the loaded application; a 5-mm trocar works just fine.
3. Stop using so many uterine manipulators.
Traditionally, some sort of uterine manipulator is used with most gynecologic laparoscopies if the patient still has her uterus. Many of these manipulators require cervical dilation and instrumentation of the uterus. But they are rarely necessary. Most tubal ligations, salpingectomies, oophorectomies, and diagnostic laparoscopies can easily be done without a uterine manipulator. If you know specifically that you are a doing a procedure that involves the posterior cul-de-sac (more than just looking at it) or a uteropexy procedure or other complex surgery that requires specific uterine positioning, then a uterine manipulator can be very useful. A uterine manipulator is also very useful for ruptured ectopic pregnancies, where elevating the uterus up and out the cul-de-sac (along with steep Trendelenburg) can allow for rapid visualization of the rupture tube. Otherwise a sponge-stick placed in the vagina serves most purposes and your patient will not have to experience the pain of having her cervix dilated and her uterus instrumented unnecessarily.
4. Give perioperative ketorolac.
A single perioperative dose of ketorolac (60 mg) reduces postoperative pain in the first four hours after surgery, reduces postoperative nausea and vomiting by half, and shortens the time to discharge. Unfortunately, many surgeons are hesitant to use perioperative ketorolac due to an unfounded fear of bleeding. Rest assured, this concern about bleeding is completely unscientific.
What else?
Don’t inject local anesthetic at the trocar insertion sites to reduce pain; this strategy, used by lots of surgeons, has been studied extensively and doesn’t work.
Using 5-mm trocar means you don’t have to close the fascia with suture, which reduces foreign-body inflammation and associated pain.
You also don’t need to close the skin with suture; Dermabond or a similar adhesive is an excellent alternative and saves times and money. Reduced time of surgery will also reduce postoperative pain.
Lastly, try to keep your insufflation pressure as low as you can, under 15 mm HG if possible. This is also associated with less pain.