A patient of mine moved out of state after her last pregnancy. She’s pregnant again and doing fine at about 12 weeks. Yes, I’m sad that she left me. But she e-mailed me recently wondering why I didn’t do a bunch of antenatal testing that her new doc says she must have. Specifically, the new doctor told her that since her BMI is above 30, she must do an ultrasound (US) at 32, 36, 37, 38, 39, and 40 weeks. She has lost some weight since before the start of her last pregnancy so she was understandably confused about why she needed this testing now but didn’t need it before. Am I the problem, or is he?
So, what gives? Well, her new doc is a greedy quack, or something like that. He may not consciously realize that he is a greedy quack; he probably tells himself lies like, “Better safe than sorry.” But that is no excuse.
There are few things as abused and over-utilized in all of medicine today as obstetric ultrasound. Every mom loves looking at her baby and every doc loves making a lot of money, so combine the two and it’s a perfect storm of unnecessary and potentially harmful testing. Women and physicians over-estimate the value and necessity of ultrasounds; both are often falsely-reassured because of a good result and falsely-alarmed by a bad result.
Let’s briefly review the ACOG-endorsed reasons to do extra antenatal ultrasounds (bearing in mind that, normally, the only ultrasounds that a low-risk, asymptomatic woman should receive are perhaps a first trimester US and then an anatomic survey in the mid-trimester).
Here are indications for fetal surveillance testing as listed in the ACOG Practice Bulletin 145:
Maternal conditions:
- Pregestational diabetes
- Hypertension
- SLE
- Chronic renal disease
- Antisphospholipid syndrome
- Poorly controlled hyperthyroidism
- Hemoglobinopathies
- Cyanotic heart disease
Pregnancy-related conditions:
- Gestational hypertension
- Preeclampsia
- Decreased fetal movement
- Poorly controlled or medically treated gestational diabetes
- Oligohydramnios
- Fetal growth restriction
- Late term or post-term pregnancy
- Isoimmunization
- Previous fetal demise (unexplained or recurrent risk)
- Monochorionic multiple gestation (with significant growth discrepancy)
There are other reasons perhaps to do antenatal testing but, in general, the following principles should be met:
- The risk of fetal demise is significantly increased above the baseline population;
- The risk of fetal demise occurs predominately in the third trimester when antenatal testing would actually occur;
- There is a predictable pattern of fetal distress that precedes fetal death which is detectable by antenatal testing.
There are some conditions where these criteria are not met entirely, like intrahepatic cholestasis of pregnancy, where no predictable pattern of distress is observed. Determining which patients meet these criteria is the subject of wide variation in practice patterns; we should remember that no quality study has ever demonstrated benefit from antenatal testing, so we tread somewhat in the realm of expert opinion for each condition. There are also no studies to indicate whether testing should be done once per week or twice weekly, and no good data that indicates whether those tests should be all biophysical profiles (BPP), all non-stress tests (NSTs), or a combination of the two.
The lack of certainty about the appropriate indications for testing creates the perfect storm for therapeutic drift: if the intervention is good for one thing, it’s probably good for another thing that is similar to that first thing. People literally make up indications for lack of something specific to do. If testing is good for cyanotic heart disease, surely it’s good for non-cyanotic heart disease too?
Even worse, many obstetricians aren’t even that thoughtful. Many don’t know the legitimate indications in the first place, and they believe testing is indicated for anyone who is “high-risk.” But what does “high-risk” even mean? Easy reimbursement and fear of litigation, plus improved patient satisfaction because she gets to see her baby and experience relief when it doesn’t die from whatever anxiety-provoking boogeyman the doctor has seized upon, add fuel to the fire of unnecessary testing.
Obstetricians, naturally, can’t stand the idea of a patient suffering an IUFD at 39-40 weeks. The only thing worse is being sued for it and an attorney arguing that it wouldn’t have happened if the patient had undergone “appropriate” surveillance (even though good studies don’t show this to be the case). These attorneys have easier cases to make when there is a false “standard-of-care” to fall back on; this is yet another reason why we should be leery of doing anything that is not science-based in the first place.
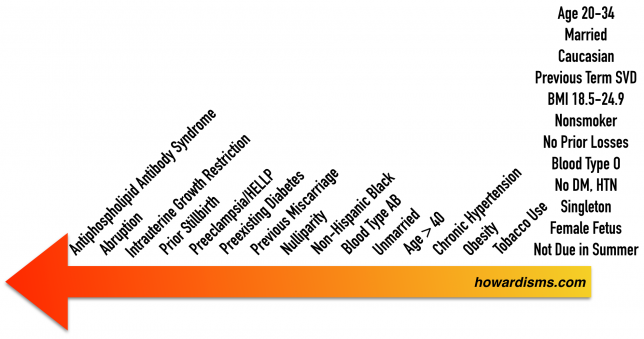
So, what is high-risk? Which pregnancy conditions and maternal conditions increase the risk of fetal demise? For my patient, we should ask, Does maternal obesity increase the risk of IUFD? I’ll go and ahead and tell you now that it does. But so does having a male fetus and being born in the summer; should patients with male children and summer due-dates also receive antenatal testing? Clearly we need to know which maternal or fetal conditions carry the greatest risk, and where the benefits of screening outweigh the risks.
What risks of screening, you ask? Well, there are many, but mostly iatrogenic preterm delivery and excess risk of maternal cesarean. There are others, and the economic consequences and psychological implications shouldn’t be ignored. But all interventions come with risk, and antenatal fetal surveillance is no exception. I recently saw a woman who had routine weekly testing in her last pregnancy; she was unsure of the reason, but her first thought was that it was because she had Medicaid. At 37 weeks, she was feeling fine and had good fetal movement but she was discovered to have “low fluid.” This led to an induction. After 12 hours of Pitocin, she had her water broken at 3 cm; she then rapidly changed to 7 cm but had some fetal decelerations associated with this and she had a stat cesarean delivery. Maybe she was transitioning rapidly and the baby had a vagal response; maybe she abrupted – I don’t know. But her cesarean and early term delivery were almost certainly a consequence of a false positive test performed without an indication.
The more the testing is over-used, the more excess harms might occur. This is the problem with every screening test, and we must be vigilant to apply the tests to the right populations who will most benefit. Harm quickly outweighs benefit when the test is misapplied.
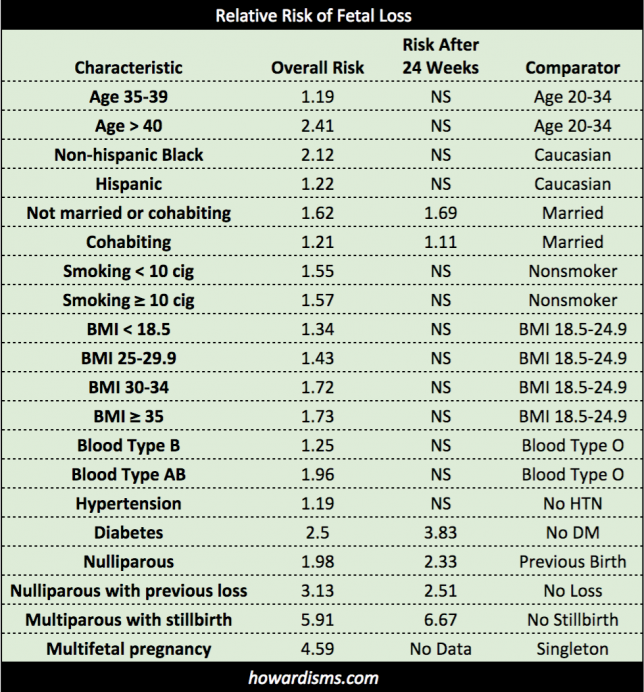
So what are the risks of various high-risk conditions? Let’s first consider pre-existing conditions; in other words, things that could be identified at the first OB visit. This article from 2011, published in the Journal of the American Medical Association, provides us with information about the risk of pregnancy loss associated with various pre-pregnancy conditions.
The first thing to note about this data is that a lot of things independently contribute to the risk of fetal loss, including Type AB blood or being black; in fact, those two factors increase the risk of loss more than obesity, being between ages 35-39, or hypertension. Despite this fact, to my knowledge, no one is doing antenatal testing just because a woman has Type AB blood.
But the second thing to note about this data is that almost all of these risks occur before 24 weeks, meaning that for most of these risk factors, antenatal testing (and subsequent indicated early delivery) wouldn’t be of any value. In fact, the only risks that persist past 24 weeks gestations are being not married, diabetes, nulliparity, previous loss or stillbirth, and multifetal pregnancy (though this study doesn’t have sufficient numbers to demonstrate the last association). Again, I am unaware of anyone who does antenatal testing on unmarried women, but that is a bigger independent risk factor than smoking, obesity, being black, age > 40, or hypertension.
Many, many reports over the years have identified risk factors for fetal demise, but be careful not to mistake overall risk (at any gestational age) with risk in the third trimester where antenatal testing might be beneficial. The greatest risks from this data are for pregnancies with previous stillbirths, pre-existing diabetes, and (likely) multifetal pregnancies, particularly monochorionic pregnancies.
Hypertension itself doesn’t increase the risk of a loss after 24 weeks, but since hypertension is associated with an increased risk of preeclampsia or intrauterine growth restriction (IUGR), then enhanced surveillance is still necessary in order to find the patients who might need testing, though this might mean only assessment of fetal growth and blood pressure checks. Nulliparity is associated with an increased risk, but no one is doing testing just because of this. Another way of thinking about the risk of nulliparity is that if a woman has already had a successful pregnancy, then her risk of loss is decreased. No history is not always a good history. But, still, that’s not a reason to do extra testing.
These are just pre-existing conditions. The study also found that none of the following were associated with an increased risk of loss:
- Advanced reproductive technology
- Previous cesarean delivery
- Autoimmune disorders
- Seizure disorders
- Hemoglobinopathy
- HIV
- Syphilis
- Hepatitis B
- Hepatitis C
- Thyroid Disorder
- Rh Negative
- Blood Type O, A
- Lifetime Drug Use
- WIC Recepient
- Low Socioeconomic Status
- Uninsured
- Maternal Education (Non-college or high school graduate)
- Adolescent
There are other maternal conditions which are rare enough to not be included in a study like this, but which nevertheless can be devastating. For example, up to 30% of women with Antiphospholipid Antibody Syndrome (APS) will experience a stillbirth.
So what about factors that develop during a pregnancy? There are several important conditions that increase perinatal risk that may occur during pregnancy, and most of these are covered in the ACOG list of antenatal testing indications. Here are a few:
- Antepartum hemorrhage (RR 3.4)
- IUGR (RR 7.9)
- Abruption (RR 10.2)
- Decreased fetal movement (RR 4-12)
- Post-term pregnancy (RR 2-4)
- Preeclampsia/Gestational HTN
- HELLP Syndrome
- Uncontrolled thyroid disease
- Rh Isoimmunization
- Cholestasis of pregnancy
- Poorly controlled gestational diabetes
There are more to be sure, but these conditions (along with preexisting diabetes) account for most of the demises among non-anomalous fetuses. The conditions with a pattern of abnormality prior to demise are those most amenable to testing. For example, IUGR usually shows clear and consistent changes that are observable with ultrasound before a demise occurs, starting with lagging abdominal circumference, then asymmetric growth restriction, oligohydramnios, cephalization, elevated systolic/diastolic ratio of the umbilical artery (UA) blood flow, absence of UA flow during diastole, reversal of flow, and then potential fetal death. This slow-developing pattern is perfect for finding a pregnancy that might benefit from early delivery.
This pattern is related to problems with the placenta, and ultrasound is useful for conditions that involve similar placental abnormalities, such as hypertensive disorders, IUGR, or post-term pregnancies. It is also good for conditions where there are structural abnormalities associated with fetal distress or observable anatomic abnormalities, like hydrops. But it useless for conditions where fetal death is sudden and unpredictable, as in the case of cholestasis of pregnancy.
Sometimes, extra testing is necessary to find the group of patients who might benefit from testing. For example, conditions that are associated with IUGR (like HTN) require at least serial observation of fetal growth and then antenatal testing when low amniotic fluid or evidence of growth restriction develops. We usually over-test this population (hypertensive women) to maximize our impact in finding women who will benefit from intervention. But we have to be careful not to create scary diseases where none originally existed, as we have done with oligohydramnios.
Oligohydramnios is one of those conditions that, by itself, does not increase fetal risk; but it may be a sign that another process might be going on which does increase fetal risk, like IUGR or placental disease. We should care about oligohydramnios only in that it serves as a bellwether of worse disease and we should monitor oligohydramnios to monitor for this worse disease. But when we believe that oligohydramnios in and of itself is bad, then we may become guilty of diagnostic drift: If a single deepest pocket of less than 2 cm is bad, then perhaps an amniotic fluid volume of less than 5 cm is bad as well. This type of drift harms patients.
But drift litters our antenatal testing practices. If poorly controlled gestational diabetes or poorly-controlled thyroid disease is bad (i.e., requires testing), then perhaps we should also test well-controlled diabetics and patients with stable thyroids? If twins with one placenta require monitoring, then perhaps twins with two placentas should be monitored as well? If a patient has an indication for growth observation, then perhaps we should throw in weekly antenatal testing too?
Soon, drift would have us testing every pregnant woman. This is clearly wrong and we need to be precise about which patients benefit from extra testing and which patients are harmed. Unfortunately, ultrasound revenue is a precious commodity of far too many obstetrical practices, and it is far too easy to order (and profit from) these unnecessary and potentially injurious tests.
The therapeutic imperative often drives us to treat one type of risk with an intervention that might be better suited for another type of risk. This is a visceral (rather than logical, evidence-based) response to an unsettling circumstance. In a mild case, we might see antenatal testing recommended for a healthy woman over age 35 (advanced maternal age), when in fact her pregnancy-related risks are almost exclusively related to decreased fecundity, higher rates of miscarriage, and increased chance of fetal aneuploidy. A biophysical profile or a nonstress test provides no information about any of these risks and those tests are wholly unrelated to the real problems; but a woman, once labeled as “high-risk” for any cause, is soon treated with any available intervention, even though the risk and the treatment are disjointed. (Maybe some magnesium while we are at it?)
In another example of such visceral transference, the cesarean delivery is seen as the panacea of all problems obstetric. Let’s “cut our way out of this mess” is the rallying call for closure anytime an obstetrician is uncomfortable with any aspect of the pregnancy or the labor, even if a cesarean is not the right treatment. Concern (visceral affectation) about a Category 2 tracing (say some occasional variable decelerations) coupled with fear that the baby might be a little big (perhaps because she had a false positive gestational diabetes screen) and some impatience because the labor is proceeding “slowly,” all adds up to a cesarean delivery; but the treatment of each of these conditions was not a cesarean delivery. If the variable decelerations were severe enough or frequent enough to be a concern, then an amnioinfusion would be in order; if there is clinical uncertainty about the size of the baby, then palpation or even an ultrasound should be performed; and a slow labor might perhaps need augmentation and patience. The sum of many small things does not always equal a big thing. But in the world of obstetrics, 1+1=cesarean delivery and all patients reckoned as “high-risk,” for any reason, equals antenatal testing.
No pregnancy is without risk, and risk exists on a spectrum.
So where do you think we should draw the line and start antenatal testing? It’s somewhere between preexisting diabetes and previous miscarriage, I’d say. If you are going to do testing on women with obesity, please make sure you also do testing on single mothers, all black patients, first time moms, and women with blood type AB since they all have greater risk than obese women.