It, unfortunately, happens that a physician who works hard to practice evidence-based medicine sometimes appear as an outlier compared to other physicians. In Obstetrics, this is most palpable when patients present who have had care with others doctors in the current or a previous pregnancy. They, naturally, compare what I do to what the other guys did. So, I’m begging folks to stop doing the following things so that I don’t look bad…
Bed rest
I have written about bed rest before and there is a lot of great writing about this topic. Here is a recent piece worth looking at. The bottom line is this: It doesn’t work (at all) and it is harmful. Don’t recommend bed rest or other vague activity restrictions for any condition in pregnancy.
Fundal heights
It is common practice for Ob/Gyns to measure the fundal height at each visit after 16 weeks or so. In theory, the measurement taken from the symphysis pubis to the “top” of the fundus in centimeters should approximately correlate to the gestational age in weeks. In other words, at 34-weeks the height should measure 34 cm ± 2-3 cm.
In reality, there is simply no scientific evidence that this measurement has any ability to predict babies that are too small, too big, or anything else. It has little intra-observer consistency, it is heavily influenced by the bias of the provider knowing how many weeks the patient is and seeing the numbers on the tape, and there is poor agreement about what the “top” of the fundus even is. There is a narrow range of women whose body habitus is amenable to an “accurate” measurement, and there is significant ethnic variation. Even the original and most cited trial that helped standardize these measurements showed no difference in fetal outcomes. It is heavily influenced by the fetal and maternal position and even how much urine is in the bladder, let alone how much the patient weighs.
Where effect has been observed for detecting fetal size abnormalities, it is in the highest risk patients, like diabetic women who should be receiving serial growth ultrasounds anyway.
Unless the same person is measuring the fundal height each time, in a double-blinded manner (not knowing the weeks’ gestation or seeing the numbers on the tape) in a normal weight woman with an empty bladder and a fetus in a longitudinal position, and charting the values on a table specifically made for the woman’s ethnicity, then fundal height is a complete waste of time and is not effective at predicting small or large babies (at least it is not any better than palpation).
The truth is, we should be screening women at risk for fetal growth abnormalities with serial ultrasound (like diabetics, those with excessive weight gain, patients with hypertension, etc) and we should palpate the fetuses of low-risk women.
It’s time for McDonald’s rule to be of historical interest only (though it is an open question whether it may be of benefit in high-risk women in resource-poor countries; not everyone can ultrasound their diabetics and hypertensives).
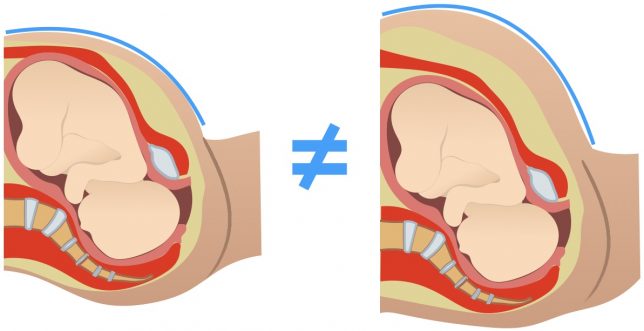
These two blues lines are not equal, though the babies are the same size. Basic geometry tells us the fallacy of fundal height measurements.
Hydration
A too common practice in triaging women with threatened preterm labor is IV hydration. Patients are commonly told that their contractions are due to dehydration, and while it is true that dehydration can cause non-labor uterine contractions, it isn’t true that dehydration causes preterm labor. More importantly, the women who come to triage complaining of contractions are almost never dehydrated, but that doesn’t stop them from getting fluid boluses.
When a woman is having contractions (at least Braxton Hicks or Caldeyro-Barcia contractions), there may be a temporary diminishment in uterine activity due to the dilution of oxytocin and the Henry-Gauer reflex. Antidiuretic hormone (ADH) and oxytocin are both made in the posterior pituitary. When the blood volume is expanded, this results in a decrease in the production of both ADH (through left atrial distention) and oxytocin (through homology), as well as a dilution of serum oxytocin levels. This artificially may lead to a diminishment of nonsignificant contractions even if the patient isn’t dehydrated, but it does nothing to stop preterm labor (also here).
It also doesn’t work as a tool to distinguish threatened preterm labor from the real thing. Worse, it is a net harm to women. Not only does it require an invasive procedure that is unnecessary (starting an IV) for most women presenting to triage with contractions and wastes precious and scarce health care dollars, it also could kill them when combined with other non-evidence-based interventions. Hydration with IV fluids can cause pulmonary edema, as can commonly-used preterm labor drugs like magnesium sulfate, terbutaline, and nifedipine. The flash pulmonary edema associated with the combination of IV fluids and magnesium sulfate can lead to pulmonary failure and ARDS. I have personally taken care of two critically-ill pregnant women in the ICU who presented to triage with non-labor preterm contractions; they received IV hydration and then when their contractions didn’t abate they received magnesium sulfate. Then they suffered pulmonary failure and both survived after weeks in the ICU (though their babies were born by Cesarean due to fetal distress due to pulmonary failure at an early gestational age).
First, do no harm. And please stop telling women that their preterm contractions were caused by dehydration, or that they should go home and “rest” and drink something. Let’s try to believe in science.
Tocolytics
Speaking of believing in science, I would also ask that you stop using tocolytics altogether. They simply do not work. I won’t spend too long discussing this here, but the short history of tocolytics goes like this: in the 1970s Fuchs showed that IV alcohol was an effective “tocolytic;” it wasn’t and no one today believes that it arrested preterm labor. It became widely used but had horrible side effects. In the late 1970s and early 1980s, two research groups showed that magnesium sulfate was equal in efficacy to alcohol and clinicians embraced this finding because it had such a better side effect profile. At the time, they believed alcohol worked. Soon, magnesium supplanted alcohol. Then, ritodrine and terbutaline were shown to be equally effective to magnesium and they became widely used as well. In time, nifidipine and indomethicin were also shown to be equal to magnesium, but not better than placebo.
In time, the first placebo-controlled trials were performed for magnesium and other emerging tocolytics. No studies showed fetal benefit with the use of tocolytics (some showed harm) and none showed prolongation of the pregnancy, even for 48 hours (one showed that the placebo group stayed pregnant longer). Eventually, we started to roll back the role of tocolytics; we stopped using them for longer than 48 hours, we used lower doses, we used them only for women who hadn’t completed steroids, and we focused on using the one with the best side effect profile because we realized that none of them worked. In fact, every meta-analysis of the literature since 1991 has concluded that all tocolytics are ineffective.
If you use them, please cite the randomized, placebo-controlled trial that states that neonatal outcomes are improved by their use. In fact, it is interesting to me personally that among the hundreds of trials done in the last 40 years and the dozens of placebo-controlled trials, there’s not even a single false positive study! I would expect 5% of them to have shown false positive results given an alpha of 0.05, but none have.
Tocoylsis is an embarrassment to Ob/Gyn and to the evidence-based practice of obstetrics. The continued use of tocolytics and the motivated reasoning that attempts to rationalize their use is perpetuated by the therapeutic imperative (we have to try something!) and a fear of liability. Ironically, we encourage liability when we promote a false standard of care and act like a treatment works that clearly does not.
Oh, and magnesium doesn’t prevent cerebral palsy either.
Unnecessary ultrasounds
A lot of ultrasounds performed during pregnancy are unnecessary. A lot. But here I was thinking of the routine practice of performing an ultrasound at around 36-37 weeks on women with uncomplicated pregnancies in order to determine fetal size and position. Please stop doing this, too. The fetal position should be determined by palpation, and palpation is also the preferred method to determine fetal size. If you discover something on palpation that needs clarification, ultrasound may be useful. In fact, I commonly see this practice leading to harm as women are talked into primary cesareans because their babies are “big” (usually just 8-9 lbs) or they are discouraged during their labors because the thought was planted in their minds that the baby is just too large. They are also frequently brow-beaten into an induction “because the baby is getting too big” which independently increases their risk of cesarean.
Unnecessary cervical exams
Finally (for today), please stop checking the cervices of asymptomatic pregnant women each week after 35-36 weeks. It just doesn’t mean anything. It doesn’t predict when she will deliver in any meaningful way and it likely leads to an increased number of unnecessary inductions of labor while causing women discomfort. Like all tests and exams, it should be done with a specific intent. If you are planning on an induction, performing a cervical exam can help inform the method and sensibility of proceeding with an induction. If a woman is having regular (under five minutes) uterine contractions, then a cervical exam can help determine if she is in labor. If she is beyond 39-weeks’ gestation and would like her membranes swept, then do it. Apart from those reasons, there really is no point in a cervical exam.