(Note: I have no personal knowledge of Serena Williams’ pregnancy or the care she received. This article is based on publicly available information only and many details are surmised.)
Serena Williams recently had a baby. Apparently, she almost died. Here’s how Serena herself described what happened:
I almost died after giving birth to my daughter, Olympia.
Yet I consider myself fortunate.
While I had a pretty easy pregnancy, my daughter was born by emergency C-section after her heart rate dropped dramatically during contractions. The surgery went smoothly. Before I knew it, Olympia was in my arms. It was the most amazing feeling I’ve ever experienced in my life. But what followed just 24 hours after giving birth were six days of uncertainty.
It began with a pulmonary embolism, which is a condition in which one or more arteries in the lungs becomes blocked by a blood clot. Because of my medical history with this problem, I live in fear of this situation. So, when I fell short of breath, I didn’t wait a second to alert the nurses.
This sparked a slew of health complications that I am lucky to have survived. First my C-section wound popped open due to the intense coughing I endured as a result of the embolism. I returned to surgery, where the doctors found a large hematoma, a swelling of clotted blood, in my abdomen. And then I returned to the operating room for a procedure that prevents clots from traveling to my lungs. When I finally made it home to my family, I had to spend the first six weeks of motherhood in bed.
I am so grateful I had access to such an incredible medical team of doctors and nurses at a hospital with state-of-the-art equipment. They knew exactly how to handle this complicated turn of events. If it weren’t for their professional care, I wouldn’t be here today.
There are tons of stories like this one. I’ve heard hundreds of women tell me the stories of why they had a cesarean in their last pregnancy and many of them had dramatic complications like Serena. Almost all of them felt thankful for the emergency care they received. They were thankful that the doctor and the nurses were able to save the babies’ lives and subsequently save their own lives. They always use the term “emergency” to describe their cesarean delivery.
This feeling that the doctors and the nurses saved the patient’s baby through heroic and emergency efforts is what I call The Serena Syndrome.
Let me explain.
Let’s look at the Serena Williams Story from my perspective.
Apparently, in 2011 Serena sustained a foot injury which immobilized her. With immobilization as her only known risk factor, she suffered a pulmonary embolism. She missed tennis for one year while recuperating. In addition to being treated for the pulmonary embolism and the foot injury, she was also later hospitalized for bleeding secondary to her anticoagulation therapy.
We can assume then that during her pregnancy she was anticoagulated, likely with Lovenox or heparin. She may have a genetic predisposition to blood clotting, but we don’t know this from the public records. In any event, she should have been prophylactically anticoagulated throughout her pregnancy.
The interesting part starts with her labor and delivery.
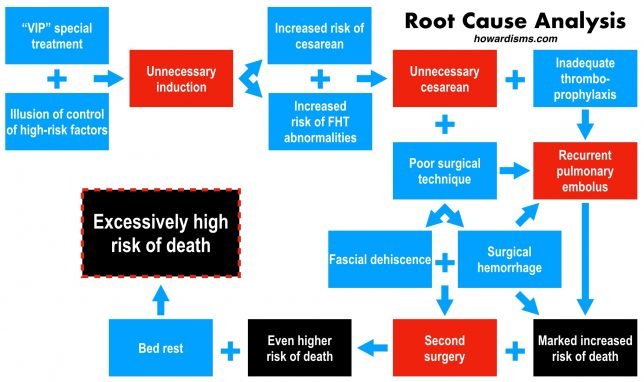
Serena was induced at a hospital in West Palm Beach, Florida. She had a whole floor of the unit to herself. I will assume that she was induced because of her celebrity status or the fact that she was on anticoagulants. Her obstetrician may have pressured her into a scheduled delivery so that the timing of stopping the anticoagulants would be easy. Or, maybe, because she was advanced maternal age, her obstetrician might have thought it best to bail at 39 weeks. Either way, she didn’t have a spontaneous labor. So this leads us to mistake #1.
Mistake #1: Induction of labor increases the risk of cesarean delivery in primigravid patients and therefore increases the risk of death; this is particularly true if the mother has a comorbidity.
Serena could have been educated to stop her prophylactic dose of heparin whenever she felt like she was having regular uterine contractions. Given the length of the latent phase of labor for most first-time moms, she easily would have had an opportunity for her prophylactic heparin to leave her system, allowing her to receive regional anesthesia if she so desired. Plus, a spontaneous labor would almost certainly be quicker than an induction of labor, which would shorten the time that she lied immobile on her back undergoing the induction. This means less time with vascular stasis and less time off her anticoagulation.
At some point, she started to have fetal heart rate deceleration with her contractions. Obviously I’ve not seen the fetal tracing, but I’m willing to bet a large amount of money that I would not have done a cesarean for whatever was going on. The one thing we know is that the “deep dips” were happening with her contractions. I assume then that these were variable decelerations occurring with her contractions. This indicates that this was likely occurring during the transition phase of labor and may have been related either to head compression or cord compression. Since the decelerations resolved after each contraction, then it is likely that with patience and appropriate resuscitation, Serena could have continued to labor and hopefully deliver vaginally. This would include not just position change but also an amnioinfusion.
Abnormal fetal heart tracing patterns are more likely to develop with inductions of labor than in spontaneous labors. Induced women often have stronger contractions, earlier amniotomy, and a longer labor than women with spontaneous labor. We don’t know the details for Serena, but we do know that the vast majority of cesarean deliveries performed for category 2 fetal heart tracings are unnecessary. That brings us to mistake #2.
Mistake #2: If there were ever a time to avoid an unnecessary cesarean, it’s in patients who are at higher risk of complications.
A black woman undergoing a cesarean delivery is at 5.5x the risk of thromboembolism as a black woman undergoing a vaginal delivery.
Serena was in the highest risk group of patients at risk for thromboembolism, even without her history of pulmonary embolism. I don’t want to do a cesarean delivery on anyone who doesn’t need one, but I in particular don’t want to do one on someone who is at an increased risk of thromboembolism after surgery as well as, paradoxically, hemorrhage due to the postoperative use of anticoagulants.
It takes a lot of work to have a low cesarean delivery rate. Read more about that here. But, obviously, if you are trying not to do a cesarean on someone, then for starters don’t induce her, especially first-time moms with unfavorable cervices; be patient with her labor, and don’t over-react to physiologically normal fetal tracings. Use an algorithm to manage labors and abnormal fetal tracings which reflects the best available evidence. Unfortunately, Serena went for the VIP experience and delivered at hospital with a cesarean delivery rate almost double of what it should be. She had her 6 lbs 13 oz baby at St. Mary’s Medical Center in West Palm Beach which has a 36% cesarean delivery rate with the second worst length of stay for cesareans in the state (over a day longer than the state average) and significantly higher cost than the state average per delivery. This suggests a high rate of failed inductions. Women need to be advocates for themselves by picking hospitals with low cesarean rates, low cost, and short lengths of stay. Of course, St. Mary’s does offer “high end amenities” and a VIP suite.
Error begets error.
When a cesarean delivery is performed late in labor on an emergent basis, the risks of complications and bleeding are drastically increased. The risk of hemorrhage is increased both from uterine atony but also from surgical site bleeding. Serena’s cesarean apparently was performed late in her labor. This means that she likely had a well-developed and thin, elongated lower uterine segment which increases the risk of tearing laterally into the uterine vessels or inferiorly into the vagina and cervix. I don’t know the details of her surgery, but I do know that if her surgeon performed a bladder flap then her risk of hemorrhage was increased even more.
There are clearly some things we can do at the time of cesarean to avoid extensions into the cervix and vagina and the lateral vessels. These things include:
- using a cephalocaudad digital dissection technique in the lower uterine segment to perform the hysterotomy,
- performing a relatively high incision in the uterus if the lower uterine segment is well developed,
- not performing a bladder flap,
- including the peritoneal edges in the uterine closure,
- and using a vaginal hand to elevate the fetal head to decrease the risk of dangerous uterine incision extensions.
I don’t know if any of these things were done or not. But I do know that Serena was taken back to the operating room two days later and had a large hematoma evacuated. I would guess that the surgery could have been performed better and that the bleeding was a consequence not of the blood thinner but of poor surgery. That leads to mistake #3.
Mistake #3. If you must do surgery on a high-risk patient, use the best techniques.
The difference in outcomes between good surgical technique and bad surgical technique isn’t noticeable in average or low-risk patients. You can get away with sloppy technique, bladder flaps, lateral dissection of the hysterotomy, non-inclusion of the peritoneum in the uterine closure, and other nonsense in the vast majority of patients. But when your patient is on an anticoagulant and has a cesarean performed late in the active stage of labor, then good technique can be the difference between life and death. If you need to brush up on cesarean technique, check this out.
We know that Serena’s symptoms of pulmonary embolism began about 24-hours after her delivery. Serena has also stated that she was not on anticoagulation at the time these symptoms began, 24-hours after delivery! In fact, Serena famously went out to the nurses station asking for a Heparin drip and a CT scan. This brings as quickly to mistake #4.
Mistake #4: If a patient needs anticoagulation, start it 6 hours after a cesarean delivery.
This is an ACOG recommendation – yet Serena was still untreated 24 hours after delivery. Is this because there was extra bleeding at the time of the cesarean and the surgeon was worried about bleeding and therefore did not resume the anticoagulation at the right time? Again, error begets error. Sloppy surgery leads to pulmonary emboli. What’s more, Serena’s coagulation cascade was likely activated even more than usual due to the excess hemorrhage at the time of surgery and postoperatively. If there were ever a time to use the best techniques and avoid excessive bleeding, it’s when your patient is at a markedly increased risk for pulmonary embolism. If taking heparin 24 hours after a cesarean delivery results in significant hemorrhage, it’s a sign that the surgery was not performed well to begin with. I depend on adequate suture bites and good knots to prevent bleeding after a cesarean, not the patient’s coagulation cascade.
When Serena went to the nurse’s station complaining of classic symptoms of a pulmonary embolism, her doctor ordered a lower extremity duplex Doppler. The physician didn’t realize or at least think about the fact that Serena’s individual risk of a pulmonary embolism was excessively high. Not only did she have classic symptoms of a pulmonary embolism, but she also was a black woman with a history of a pulmonary embolism who just underwent a major surgery with excessive hemorrhage after being strapped down in a bed for 24-hours. Ordering a Doppler was insane. The only thing worse that could have been done was ordering a D-dimer. Thus, our next mistake.
Mistake #5. Consider the context of your decisions. Pretest probability matters.
If a patient has an excessive risk of thromboembolism based on history and physical, order the right test. If a patient is at an excessive risk of thromboembolism based on history and physical, don’t induce her labor unnecessarily and don’t withhold her anticoagulation against the recommendation of our clinical guidelines.
The day after Serena was started on Heparin to treat her new pulmonary embolism, she was taken back to the operating room because her incision “busted open” supposedly due to her coughing. I will be bold and state that no cough has ever busted open any incision I’ve ever made. Her incision didn’t bust open due to coughing, her incision busted open due to poor surgery. It’s not clear from the public records whether this was a skin dehiscence with a superficial hematoma or a fascial dehiscence with a subfascial hematoma, but both are unacceptable. Serena says the hematoma was in her abdomen, so I assume that her fascia opened up.
The last thing you want to do is take a patient who was just diagnosed with a pulmonary embolism back to the operating room to redo the original botched surgery that led to the pulmonary embolism in the first place. If this was a fascial dehiscence, then the situation is even worse then I am making it out to be. Fascial dehiscence and evisceration carries a high mortality rate (up to 25%). If it were merely a skin dehiscence with a superficial hematoma, then a return to the operating room was unnecessary and only increased her risk of thromboembolic complications further. In other words, either there was a return to the OR due a fascial dehiscence, which means that the original surgery was very poor, or there was a return to the OR due to a skin dehiscence which means that the decision-making skills of the surgeon was very poor. So,
Mistake #6 Don’t make a bad situation even worse by freaking out and making bad decisions.
I obviously don’t know the details of what actually happened. But all of this is scary. Many physicians are prone to overreact and over-intervene, particularly when they feel a little responsible for what has happened. Remember, the job is to “First do no harm.” This means doing the least invasive interventions to gain the most benefit. If this were a skin dehiscence only, then the decision to return to the operating room is dramatic and ill-advised. If it were a fascial dehiscence, then it’s another example of poor surgery. The suture bite on each side of the faccia should include 1 cm of tissue. Most people don’t do this correctly. Most people get away with sloppy surgery until their surgery is tested by complicated patients.
The last detail of this saga is perhaps the most striking. Serena apparently was instructed to spend the next 6 weeks at home on bed rest!
Mistake #7: Don’t tell people who are at high risk of thromboembolism to be on bed rest.
This is an absolutely incredible and inexcusable recommendation. This type of inactivity is apparently what led to Serena’s first pulmonary embolism after her foot surgery. Few things could have increased the risk of Serena’s death as much as this last mistake. I won’t even begin to try to justify why her physician might have asked her to do this. If anything, it confirms my suspicion that most of Serena’s problems where iatrogenic. This brings us to the last mistake and the defining feature of The Serena Syndrome.
Mistake #8: You don’t get credit for saving a mom and baby when you’re the one who almost killed both of them.
I admittedly get frustrated when I hear stories from my patients about their prior experiences. What frustrates me the most is that many of them believe that the poor care they received was necessary and life-saving. They suffer from The Serena Syndrome. A patient will tell me how she was stuck at five cm for 2 hours or how her doctor thought her pelvis was too small so she recommended a cesarean for her 8 lbs baby. She will tell me about how the baby wasn’t tolerating labor and when I request records I discover that there was moderate variability with a few variables but it was close to 5 o’clock on a Friday and she was only 7 cm. I see patients who were only allowed to push for 45 minutes; patients who were told they had to have a cesarean because they had twins; patients who were induced at 39 weeks for no medical reason at all and who eventually underwent a cesarean for “failure to progress” (a term we no longer are allowed to use by the way). Most of these patients also had at least a casual comment made to them that the baby wasn’t “tolerating labor.” These attitudes lead to maternal and fetal harm and are the primary reason why maternal mortality continues to climb.
Let’s fight the epidemic of The Serena Syndrome.
Error begets error. The best way to avoid problems is not put yourself in a position to have them.
Postscript: Most of the attention in the media about the Serena Williams story focused on her story as being an example of racial disparities in obstetric care. In the US, black women are much more likely to die during delivery than white women. I will add this to the conversation: Black women are 50% more likely to have a cesarean delivery than white women. Talk amongst yourselves now.