The financial consequences of poor prescribing habits, as detailed in Which Drug Should I Prescribe?, are simply enormous. Recall that just one physician, making poor prescribing decisions for only 500 patients, could unnecessarily add nearly a quarter of a billion dollars in cost to the healthcare system in just 10 years. In the case of prescribing habits, physicians personally gain from their poor choices only by receiving adoration from drug reps along with free lunches and dinners. But what about other treatment decisions? How much cost is added to the system when physicians deviate from evidence-based practice guidelines, and is there a financial benefit to them for doing so?
Let’s look at a practical example.
Imagine a small Ob/Gyn practice with four providers. The four providers see 1,000 young women a year between the ages of 17-20 who desire birth control (that is, each physician sees 250 of these patients). The evidence-based approach to treating these patients would be to give them a long-acting reversible contraceptive (LARC) and to not do a pap smear (of course, they should still have appropriate screenings for mental health, substance abuse, etc. as well as testing for gonorrhea and chlamydia and other interventions as needed).
If each of these women presented initially at age 17 or 18 desiring birth control and received a three-year birth control device (e.g, Nexplanon or Skyla), then it is likely that a majority of them would not return for yearly visits until the three year life of the birth control had passed. It is also likely that only 1-3 of the 1000 women would become pregnant over the three year period while using a LARC. Gynecologists for decades have tied the pap smear to the yearly female visit. As a consequence, most young women, when they learn that they don’t need a pap every year, don’t come back for a visit unless they need birth control or have some problem.
The most common need, of course, is birth control. But when women have a LARC and know that they don’t need a yearly pap smear, they are even less likely to return just for a screening visit. Admittedly, gynecologists need to do a better job of “adding value” to the yearly visit and focus on things that truly improve the quality of life for patients – like mental health and substance abuse counseling – but these things take time and it’s much quicker just do an unnecessary physical exam and move on. Physicians use the need for a birth control prescription – and the lie that they need a pap smear in order to get a prescription for birth control – in order to force women back to the office each year. What’s worse, many young women don’t go to a gynecologist in the first place for birth control because they do dread having a pelvic exam; they then become unintentionally pregnant after relying on condoms or coitus interruptus.
In the following example, the evidence-based (EB) physician sees an 18-year-old patient who desires birth control; he charges her for a birth control counseling visit and charges her for the insertion of a Nexplanon, which will last three years and provides extraordinary efficacy against pregnancy. He sees her each year afterwards for screening for STDs and other age-appropriate counseling, but he does not do a pap smear until she turns 21.
The non-EB physician sees the same 18-year-old patient who desires birth control and prescribes a brand-name birth control pill (at an average cost of $120 per month and with an 8.4% failure rate). He insists that she first have a pap smear since she is sexually active and he plans to continue doing pap smears each year when she returns for a birth control refill. He tells her scary stories about a patient he remembers her age who was having sex and got cervical cancer but thankfully he caught it with a pap smear (of course, that patient didn’t have cervical caner – she had dysplasia – but these little white lies are common in medicine). He doesn’t adequately screen her for mood disorders, substance abuse, or other issues relevant to her age group, but he does make a lot of money off of her; and he could care less about the psychological harm he might have caused her with his scary stories.
About 30% of women in this age group will have an abnormal pap smear if tested, and about 13.5% would have a pap smear showing LSIL, HSIL, or ASCUS with positive high risk HPV. The non-EBM physician would then do colposcopies on these 13.5% of women, along with short interval repeat pap smears (e.g, every 4-6 months) on the women with abnormal pap smears. About 15% of the women who receive colposcopy will have a biopsy with a moderate or severe dysplastic lesion, and the non-EBM physician will then do an unnecessary and potentially sterilizing LEEP procedure on those patients.
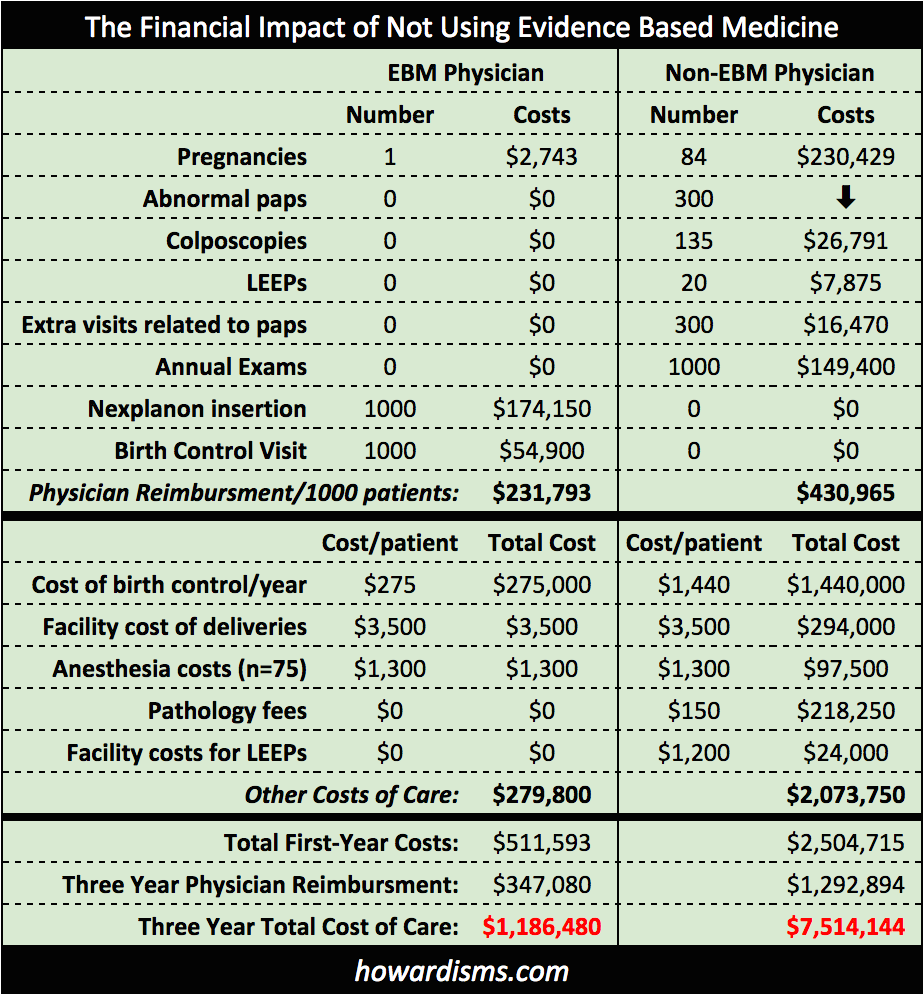
Since he gave these women birth control pills, 84 of the 1,000 patients will become pregnant each year, and this will lead to significant costs for caring for these pregnant women and delivering these babies. In fact, 252 of the 1000 women will become pregnant over the next three years (compared to 1-3 women who received a LARC). Ironically, the very reason why the patients came to the doctor in the first place is the most neglected, with nearly 1 in 4 becoming pregnant because of the poor decisions of the non-EB physician. The chart below shows the financial repercussions for the first year of care for these patients and for three years of care (since that is the useful life of a Nexplanon or Skyla LARC):
The differences are dramatic: the evidence-based physician has perhaps 3 pregnancies per 1000 patients and no issues with pap smears since none were done. I have no doubt that many of the women returned dissatisfied with the Nexplanon and some likely discontinued and switched methods, and I have allowed for return visits each year. A greater number of women who received birth control pills will return with problems and a desire to switch. But over 3 years, 252 of the women who were given birth control pills will become pregnant.
These young women came to get birth control and were instead victimized. The effects of unintended pregnancy on young women are profound. Women who have children under age 18 are nearly twice as likely to never graduate high school, nearly two-thirds live in poverty and receive government assistance, three-quarters never receive child support, and their children grow up underperforming in school. These are dramatic societal costs that must be considered a consequence of physicians ignoring evidence-based guidelines.
So what about the money? The physician who follows evidence-based guidelines will collect about $350,000 over the three year period; whereas the physician who does not will collect nearly $1.3 million in the same time. The physicians are financially incentivized to hurt young women. These extra monetary gains for the physician cost our healthcare system nearly 6.3 million dollars more. This story can be repeated for a variety of other medical problems in every speciality.
Another Ob/Gyn example: a physician who treats abnormal uterine bleeding with a hysterectomy when a lesser alternative might have sufficed (such as a Mirena IUD, birth control pills, or an endometrial ablation). The physician is financially incentivized to perform a hysterectomy because her fee is higher for that service compared to other, more appropriate services; but in order for the physician to make a few hundred dollars more, the healthcare system is drained of many thousands of dollars (the hospital charges for a hysterectomy can be enormous) and the patient is exposed to a higher risk procedure when a lower risk intervention was likely to work just as well.
The current model of financially incentivizing physicians to provide as much care as possible (what is called fee for service) is bankrupting our healthcare system and harming patients with too many interventions, too many prescriptions, and too much care. No good alternative to this system has been proposed. But fee for service provides no incentive for physicians to choose lower cost treatments, to prescribe less expensive drugs, or to perform expensive interventions only when truly needed. No good alternative to fee for service has been proposed, but every important player in healthcare realizes that the model needs to be changed in order to improve the quality of care and reduce costs.
The financial services industry faces a similar crisis. Currently, most financial advisors make money off of selling products, collecting fees for the transactions they conduct and the financial products that they sell, and, in some cases, residual fees from future earnings. This incentivizes advisors to sell products (stocks, bonds, equities, etc.) that produce the largest fees or the biggest return for them, not for the client. New federal rules are attempting to address this problem by requiring financial advisors to comply with fiduciary standards, meaning that they must put the clients’ needs above their own. How is this incentivized? A fiduciary advisor makes more money only if the client does; the fiduciary rules outlaw transactional fee (like selling an investment product) and instead tie the advisor’s fees to future client earnings. Full disclosure of conflicts of interest are also required. Essentially, the financial services industry is transitioning from a fee for service model (how many investment products can I sell?) to a fee for better outcomes model (I’ll only make more money if my client does).
In theory, physicians should comply with fiduciary rules for patient care because of our professional oath; doing what is best for patients without exploiting them is the most essential ethic of any medical professional. But professionalism among medical doctors is a true rarity, and the proof of this is the vast majority of physicians who choose the unethical approach of rejecting evidence-based guidelines and instead exploiting patients for financial gain.
Now I’m not suggesting that most physicians who don’t follow evidence-based guidelines do so because they have consciously chosen to financially exploit the patient, but in the example above of a 1,000 patients in a four physician group, if those physicians choose to follow evidence-based guidelines, they would likely not need the fourth physician and they wouldn’t be able to pay her. The finances of medical practice dictate far too many decisions, and sometimes this influence is subconscious (though many times it is not). Physicians are smart, and they are too good at couching their decisions to over-utilize interventions as if it’s a benefit to those patients: it’s never because physicians want to make more money doing it, it’s always because they are doing what’s best for patients. But the example above, which is typical for similar issues in many specialities, shows that outcomes are not better and the cost of not following evidence-based guidelines are extraordinary.
Physicians need to be financially incentivized to follow ethical, fiduciary principles. The Hippocratic Oath isn’t cutting it. Financial services advisors under fiduciary guidelines are paid more only if the client does well, and so too doctors should make more money only if their patients do well. In a $55 visit, I can choose to prescribe an inexpensive generic drug for a problem (at a cost of $48 a year) or I can choose to prescribe an expensive branded drug (at a cost of $4200 a year). Insurance companies need to recognize this and reward the physician who makes good decisions. It is much better to pay the physician another $100 to have the time to talk to the patient and educate her than it is to pay $4200 a year for the poor decision. Why not pay physicians as much for IUD insertions as they are payed for hysterectomies? Yes, I am quite serious. You would see so many IUDs being inserted that it would make your head spin, but the cost of healthcare overall would drop dramatically and patient outcomes would improve. High school graduation rates would increase. Poverty would decrease. Paychecks would go up as less money was spent on health insurance premiums. Why not pay more for vaginal deliveries than cesarean deliveries? In general, paying more for the good care that physicians provide and less for the bad care physicians provide is the solution. But what is good care and what is bad care? That’s the struggle.
I suggest three things.
- First, the total cost of care for a diagnosis, including pharmacy costs, must be part of the equation. Less expensive care must result in financial gain for the doctor (and the hospital if appropriate).
- Second, adherence to evidence-based guidelines must result in financial benefit, and deviations from EBM must be explained in detail before it’s payed for by the payor.
- Third, physicians must be financially rewarded for improved patient outcomes over a long term.
A physician who does 10 hysterectomies per year should, in most cases, be paid more than a physician who does 100 hysterectomies per year. The number of unnecessary surgeries and interventions in all disciplines of medicine is staggering, and it results in high-cost, low-quality healthcare that is bankrupting the US system. I wish that the Hippocratic Oath were enough and that physicians always did what was best for their patients even if it meant making less money, but this wish is a pipe dream. We need appropriate financial incentives.