At the 2016 ACOG Annual Clinical Meeting, a colloquia session debate was presented entitled: If No Elective Inductions Before 39 Weeks, Why Not Induce Everyone At 39 Weeks, featuring Charles Lockwood and Errol Norwitz, two well-respected thought leaders in OB/GYN. Norwitz, in particular, has been a favorite of mine for years since hearing him make the case for ending all pregnancies at no later than 41 weeks (rather than 42) several years ago. The debate can be watched at the link above, and I encourage anyone who is seriously interested in this issue to do so, but only if you promise to finish reading this later. I will summarize their points briefly here, however.
The promised “debate” between the two men turned out to be no debate at all. They did not pick a side and argue; they both reviewed some of the same, recent literature and came up with the same, questionable conclusion: No woman should continue her pregnancy beyond 39 weeks. This opinion is based on two assumptions:
- First, that pregnancies that go beyond 39 weeks face a continued and perhaps increasing risk of intrauterine fetal demise (IUFD).
- Second, that there is no benefit to the fetus or mother in continuing the pregnancy beyond 39 weeks.
This is the same logic I remember hearing so eloquently from Dr. Norwitz a decade ago, except the gestational ages were 41 and 42 weeks, respectively. The two men argue that, today, with new evidence about the risks and benefits of the proposition, the numbers should be changed and every woman should be delivered no later than 39 weeks. Both men predicate their opinions on recent statistical analyses that they feel tip the scale in favor of the earlier induction. Well, what should we do?
This is a complex topic and, unfortunately, it is a little laborious to answer. I will address this issue in three parts. In Part 1, we will consider the potential harms to women through increasing the cesarean section rate with earlier inductions. In Part 2, we will consider the potential benefits of reducing the number of IUFDs. In Part 3, we will tie it all together and consider some ancillary issues.
Part 1
Statistical commentaries, whether in studies, analyses of the literature, or just opinions, like those rendered in this debate, are often dangerously misleading if the compared groups are not matched appropriately or if all of the potential outcomes are not included. Even rare outcomes can be viewed as “statistically significant” if there is a large enough sample size. That doesn’t mean, however, that the finding is clinically significant or not otherwise trumped by some unintended consequence or outcome. The benefits and harms should be framed in terms of number needed to treat (NNT) and number needed to harm (NNH) so that we can better understand the potential for benefit and the potential for harm when we consider making a change to our practice.
For example, in this debate, there are relatively few maternal harms considered by the debaters because it is taken for granted by both men that there will be no increased risk of cesarean delivery with induction at 39 weeks compared to induction at 41 weeks, particularly for women with unfavorable cervices. This is not based on solid data. Even a slight increase in the risk of cesarean delivery would dramatically change the risk-benefit ratio. So understanding this point is very important. Let’s look at some of the available data about induction and the risk of cesarean delivery.
- Maslow et al in 2000 found, after reviewing 1,135 nulliparous women with low-risk, singleton, vertex pregnancies, that elective induction of labor (IOL) was associated with a 2.4x higher risk of cesarean delivery when compared to women in spontaneous labor, as well as increased cost and hospital time.
- Lee et al in 2015 found, after reviewing 1,375 pregnancies, a risk of cesarean of 17.3% in induced women compared to 5.3% in women who presented with spontaneous labor. This increased risk was confounded by many risk factors, including nulliparity and lower Bishop scores.
- Vrouenraets et al in 2005 found, in a prospective study of 1,389 women, a cesarean delivery rate of 12% among women in spontaneous labor compared to a rate of 23.4% among women induced for medical reasons and 23.8% among women induced electively.
- Seyb et al in 1999 found, in a prospective cohort study of 1,561 women, a cesarean delivery rate of 7.8% among women in spontaneous labor compared to a rate of 17.7% among women induced for medical reasons and 17.5% among women induced electively.
- Prysak et al in 1998 found, in a retrospective case-control study of 461 pairs of women, a 1.81-fold increased risk of cesarean delivery among women who were electively induced, with an even higher risk among nulliparous women (OR=6.14).
- Rattigan et al in 2013 found, in a retrospective analysis of 807 women, that women who had elective inductions had a cesarean delivery rate of 41.1% compared to 9.9% for women presenting with spontaneous labor.
- Vahratian et al in 2005 found, in a single institution review of 2,200 women, that elective induction in women with unfavorable cervices increased the risk of cesarean delivery by 3.5-fold.
- Luthy et al in 2004 found, in a single institution cohort study of 3,215 term, singleton, cephalic nulliparous pregnancies, a 1.78-fold higher risk of cesarean delivery with elective induction.
- Levine et al in 2014 found, in a retrospective cohort study of 862 women, a cesarean rate of 23% in induced women, compared to a rate of 7% in spontaneous laborers.
- Ehrenthal et al in 2010 found, in a retrospective cohort study of 7,804 women, that elective induction increased the risk of cesarean by 1.93-fold in nulliparous women.
Well, I could go on listing study after study like these, but for the sake of brevity I have to stop myself. The studies just listed, of nearly 22,000 women, employ a variety of methodologies and take different approaches to controlling for confounding variables, but they all agree that elective induction of labor, particularly among nulliparous women with unfavorable cervices, significantly increases the risk of cesarean delivery. So why did our debaters say that there was no increased risk? The answer is largely because of one study published in November, 2015 by Saccone and Berghella in the American Journal of Obstetrics and Gynecology (in fairness, there are other, similar published metaanalyses or systematic reviews).
In this metaanalysis of five randomized controlled trials (RCTs) involving 844 women, the authors compared multiple outcomes, including risk of cesarean, between a group of women electively induced and a group of women who went into spontaneous labor. They conclude that the rate of cesarean delivery is “similar” with a rate of 9.7% in induced women compared to 7.5% in controls. Since they only included RCTs, they did not consider the bulk of the published evidence, including any of the studies listed above. In fact, out of 1,580 possible papers considered for inclusion, all but 5 were excluded for various reasons, including 11 other RCTs which failed to meet some criteria. So here are the five, with the number of patients for each and the cesarean delivery rates:
- Cole et al, 1975: 228 women, induced: 4.5%, expectant management: 7.7%
- Martin et al, 1978: 184 women, induced: 4.3%, expectant management: 1.1%
- Tyllskar et al, 1979: 84 women, induced: 2.3%, expectant management: 2.4%
- Nielsen et al, 2005: 226 women, induced: 6.7%, expectant management: 7.8%
- Miller et al, 2014: 162 women, induced: 30.5%, expectant management: 17.5%
So these five trials were included because they were the only ones that met the author-selected criteria – out of hundreds of potential papers, the vast majority of which conclude that there is a higher section rate with induction. Among these five papers, three are from the 1970s, when the total cesarean rate was substantially lower than what is seen in modern obstetrics. It is irrelevant to include studies that have little relationship to modern obstetric practice or standards of care. They are only relevant to an obstetrician who has a sub-5% cesarean delivery rate.
The most recent paper, from 2014, in fact shows a 1.74-fold higher risk of cesarean with induction, similar to many of the papers previously cited. The remaining paper, from 2005 by Nielsen et al, showed a similar rate of cesarean but only included women who had favorable cervices. So only one study, written in the last 35 years, is even relevant to induction of nulliparous women with unfavorable cervices and it concluded that induction was associated with a 1.7-fold increased risk of cesarean. Yet, the authors boldly conclude that “induction of labor in asymptomatic and uncomplicated singleton gestations at full term is not associated with increased risk of cesarean delivery…” This type of analysis is an example of the most inappropriate use and application of statistical techniques; it perverts and frustrates the legitimate application of evidence based medicine.
From a Bayesian perspective, we must consider the totality of evidence, especially when there is only one applicable RCT performed in the last 30 years (which agreed with the traditional view that induction nearly doubles the risk of cesarean). Yet even this paper, by Miller et al, has a carefully worded conclusion: “Elective induction after 39 0/7 weeks of gestation compared with expectant management of pregnancy did not double the rate of cesarean delivery.” This smacks of sophistry; yes, it did not double the risk, it raised it by 1.7-fold. But let’s not act like raising the risk of cesarean delivery from 17.5% to 30.5% is not clinically significant. The carefully worded conclusion reflects an underlying bias of the authors. A more appropriate conclusion might have been, “Elective induction after 39 0/7 weeks of gestation compared with expectant management of pregnancy is associated with a 1.7-fold increased risk of cesarean delivery.”
Nevertheless, our debaters, with no more insight than this, accept the canard that induction of labor does not increase the risk of cesarean delivery. Granted, virtually no study done is methodologically perfect. Also, there are a few studies that show an equivalent or even lower risk of cesarean delivery with induction, though most of these studies relate to induction at 41 weeks rather than 42 weeks and/or involve women with favorable cervices. Still, the overwhelming bulk of the evidence indicates that there is an increased risk of cesarean with elective induction, particularly with women with unfavorable cervices or nulliparous women. With an increased risk of cesarean comes an increased risk of maternal harm, which our debaters have totally neglected.
I would also point out that these studies about risk of cesarean with induction are fundamentally addressing the wrong questions. The questions should be, Why are the cesarean rates so high in the first place? How many mothers are dying because of this high cesarean rate? Consider these facts:
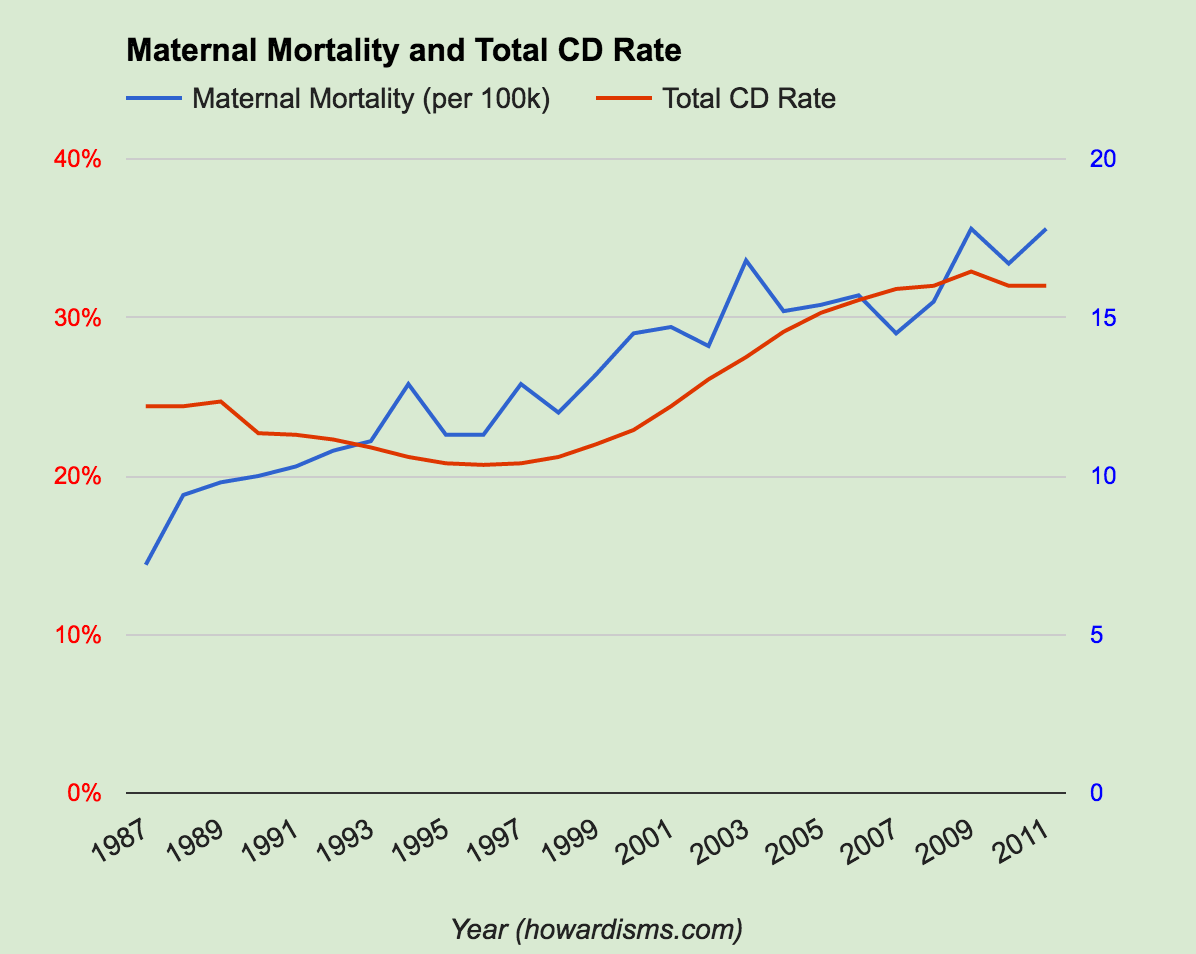
- The CDC reported a total cesarean delivery rate of 32.8% for 2012, with a primary cesarean rate of 21.5%.
- In 1996, the total cesarean delivery rate was 19.7% with a primary cesarean rate of about 15%.
- In 1996, the number of pregnancy-related deaths in the US was about 11.3/100,000.
- Pregnancy-related deaths have risen to 17.8/100,000 by 2011. This rate has been rising since the late 1980s, after more than 200 years of continuous decline.
In other words, as the cesarean delivery rate has risen 66.5% from 1996-2012, the maternal mortality rate has risen 57.5% in roughly the same time period. About 700 women die each year in the US of pregnancy-related causes, compared to about 450 women in 1996. There were less than 300 such deaths in the late 1980s. So at a time when we should be lowering the cesarean rate to save the lives of hundreds of women per year, instead our thought leaders are encouraging more cesareans.
It is nearly impossible to estimate how much higher the cesarean rate might be if we started delivering everyone at 39 weeks. Very few VBACs would happen as providers would choose not to offer women inductions who have had previous cesareans. It is unlikely that the cesarean delivery rate would only increase by around 1.7-fold, since few doctors will act like the doctors did in the controlled studies that give us numbers like that. The debaters rightly pointed out that their math only works if Ob/Gyns will be responsible and judicious in their use of primary cesarean delivery. But the average Ob/Gyn in the US already has too high a section rate and their practices are steeped with bad habits that contribute to this.
How many Ob/Gyns are actually following the principles outlined in the Obstetric Care Consensus Paper Safe Prevention of the Primary Cesarean Delivery? For example, defining active labor as starting beyond 6 cm rather than 4 cm; defining active phase arrest as no change for 4 hours rather than 2 hours; universally offering external cephalic version; not recommending cesarean unless the estimated fetal weight is greater than 5,000 g (or 4,500 g in diabetics); or not sectioning women because of a prolonged latent phase; etc. Until we are all universally following these and other evidence-based labor management guidelines, it is impossible to estimate what the “average Ob/Gyn” will do when given license to induce/deliver every woman at 39 weeks. Rest assured that many Ob/Gyns, who for years have induced women early for their own convenience, are now bathing in self-justifying glory after hearing of this Debate, and rather than avoid elective induction before 41 weeks, as the Consensus Paper recommended, they will dig in even more.
With the virtual elimination of VBACs and an even modest rise in the rate of primary cesarean, it is easy to believe that the cesarean rate would quickly approach 50%, as Dr. John Queenan in August of 2011 sagely predicted. He opined, in an editorial in the Green Journal, that without intervention, we would soon be headed to a greater than 50% cesarean delivery rate even without the help of routine 39 week deliveries. Compared to 1996, this would mean an excess maternal mortality rate of perhaps 575 women per year, assuming linear growth (I say assuming linear growth because with increasing rates of invasive placental disease, the growth rate of maternal mortality will likely be sharper). And by the way, no amount of sophistry or statistical sorcery will change this fact: The maternal mortality rate is 3.6/100,000 with a vaginal delivery and 13.3/100,000 with a cesarean delivery. Mortality, of course, is just the tip of the iceberg. Other major maternal morbidities will skyrocket, including near death events like massive hemorrhage or amniotic fluid embolism.
Ok, so the next question: Is it worth killing more and more women in childbirth? What are the benefits to perinatal morbidity and mortality? How many babies are we going to save at the expense of these maternal deaths? And should we weigh the life of a mother equally with the life of an unborn baby? We will address this question in Part 2.