One of the most common and important jobs of an Ob/Gyn is to prescribe effective birth control. Unfortunately, more often than not, the choice of birth control prescribed is wrong. There are many options for birth control but not a lot of understanding on the part of providers, or patients, about the pros and cons of each method. As with any medical issue, providers get stuck in a practice pattern and usually have a “go-to” choice of birth control that they prescribe, with two or three back-up options for special situations. These practice patterns are heavily influenced by pharmacy sampling and advertising. Despite widespread utilization and availability of birth control options, about 50% of pregnancies in the US are unintended. Half of the women who have an unintended pregnancy, that is 1 in 4 pregnancies, were using birth control at the time of conception. Almost always, the method utilized was not appropriate. Few patients are appropriately counseled about the failure rates of various methods.
So what birth control should we prescribe? Let’s try to answer this question in a more objective, evidence-based manner.
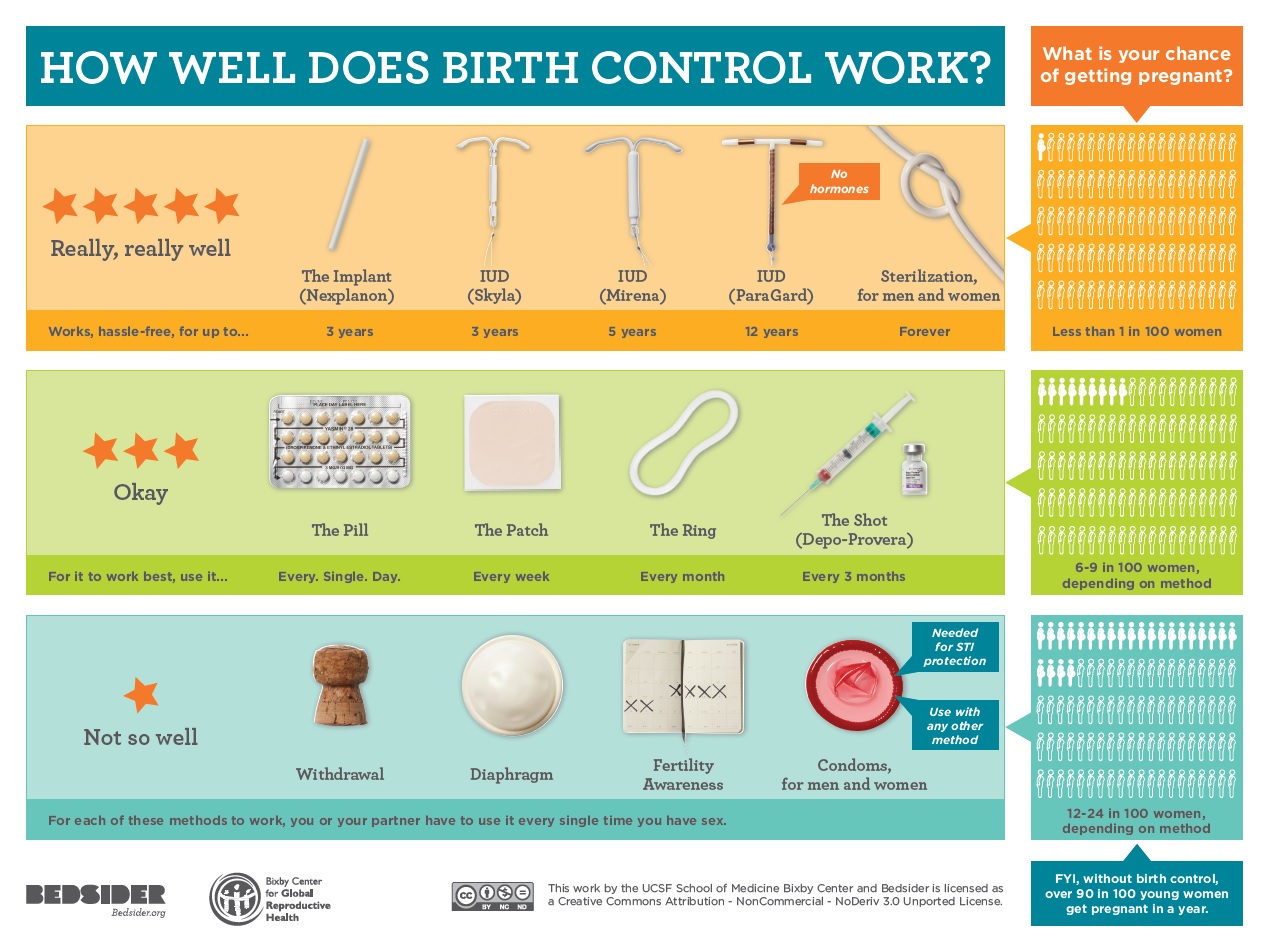
When thinking about birth control or discussing it with patients, it is incredibly useful to categorize the options into 3 tiers. Below is an outline of the 3 Tiers:
- Tier 1
- Intrauterine Devices
- Mirena
- Skyla
- ParaGard
- Implant
- Nexplanon
- Sterilization (female and male)
- Intrauterine Devices
- Tier 2
- Combined oral contraceptive pills (OCPs)
- Dozens of products
- Birth control vaginal ring
- NuvaRing
- Birth control patch
- Ortho Evra and generics
- Shot
- Depo-Provera
- Minipills
- Progesterone-only pill
- Combined oral contraceptive pills (OCPs)
- Tier 3
- Condoms
- Withdrawal method
- Spermicides
- Fertility awareness-based methods or natural family planning (NFP)
- Sponge
- Diaphragm
If you want to stop reading now, I will go ahead and tell you that Tier 1 is better than Tier 2 and Tier 2 is better than Tier 3. But Tier 1 is best not just because of efficacy, but also because of patient satisfaction, cost, mortality, morbidity; what’s more, the Tier 1 options have the fewest contraindications. These facts surprise many providers, who either don’t know them or don’t believe them; less than 10% of eligible women in the US use a reversible Tier 1 method (which is called long-acting reversible contraception, or LARC). So let’s look at the data for each of these claims.
Failure Rates
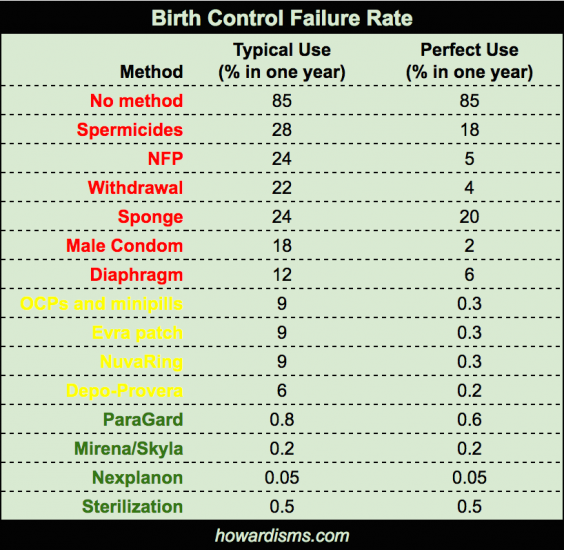
Failure rates are fairly straightforward. Of course, each year of use increases the total chance that a patient on the method will become pregnant. Here is an interactive graph that allows a patient to see what her failure rate will be over several years of using a particular method. For example, 38% of women who use the pill, patch, or ring over 5 years will be pregnant versus less than 1% will be pregnant who used a Mirena IUD in that same five year period. Or, 17% of women who use Depo-Provera will be pregnant over 3 years of usage compared to less than 0.5% of women who use Nexplanon over that same time period. Sounds crazy? It’s not. This is why at least 1 in 4 pregnancies occur “accidentally” while on birth control in the US.
Many providers either don’t tell patients the failure rates of the chosen method or, if they do, they tell them the “perfect use” failure rates. Perfect use failure rates are not clinically important. They exist in trials only. The typical use failure rate describes women who start and continue to take birth control as directed. It describes our actual patients. It is true that typical use rates vary. For example, among adolescents, the typical use failure rate of OCPs is higher, perhaps 12%, but even among the most responsible groups of patients, the failure rate is never reported lower than 2.2%. The average is 8.4% (rounded to 9% in the dataset above). Most patients feel betrayed when they learn the true failure rates of their chosen method for the first time.
Also note that the failure rate of female sterilization is higher than the failure rate of LARCs (except ParaGard). Sterilization failure rates vary with method, but even the best methods still have a failure rate of about 0.2%. Sterilization failure rates are also higher the younger the woman is. A 20-year-old woman has a significantly higher rate of failure than a 40-year-old woman (since she has more opportunity for the procedure to fail).
Many factors contribute to the efficacy of a birth control method. Most providers are shocked to see a 6% failure rate for Depo-Provera; but because patients so dislike the method there is a high discontinuation rate. So how well a patient likes a method is important, and largely governs how likely they are to continue the method.
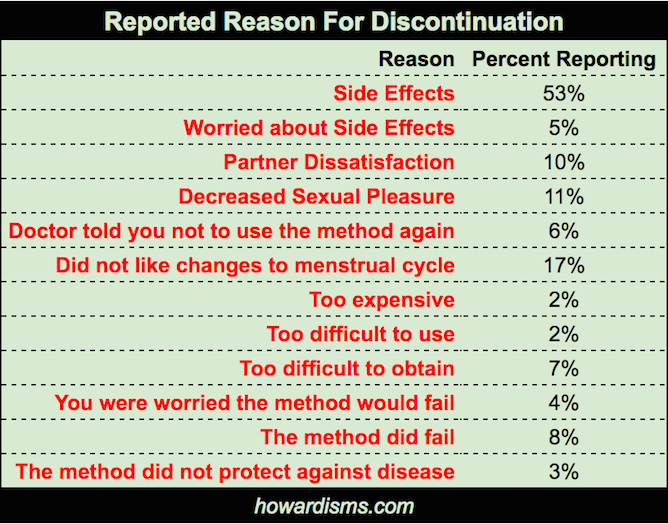
Satisfaction and Continuation Rates
Note that the medicated IUDs (Mirena and Skyla) have the highest continuation rate and the lowest dissatisfaction rate, while the patch has the highest dissatisfaction rate and the second lowest continuation rate (behind only to Depo-Provera). Patient satisfaction is clearly linked to continuation of the method, and continuation of the method is a large part of efficacy. Many providers believe that their patients will not like Tier 1 methods due to the nature of insertion or placement; yet the exact opposite is true. Patients have far fewer negative side effects with LARCs than with Tier 2 choices, and the 1-2 minutes of discomfort with insertion is minor (if you find that your patients are having more insertion-related pain and complications than this, you may need to refer them to someone else for insertion).
So why do patients tend stop their method of birth control?
The LARCs, and IUDs in particular, mitigate many of these side effects: worry about failure or actual failure, decreased sexual pleasure, and the big “side effects” category which is a catch-all mostly related to systemic hormonal changes, including everything from excessive weight gain to moodiness.
How about safety? Due to social media and harmful lawyer solicitation commercials, many patients (and providers) are worried about the safety of birth control, and of LARCs in particular.
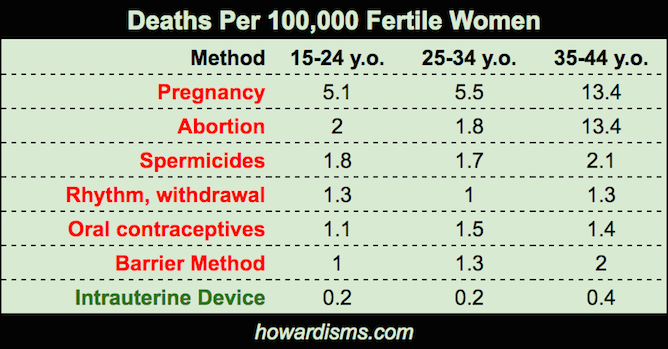
Mortality Rates
Birth control pills have always been known to cause potentially fatal complications, such as pulmonary emboli, but we have always justified these rare deaths because the risk of death with birth control pills was still almost 5 times lower than the risk of death in pregnancy. However, the risk of death with an IUD is 25+ times lower. Obviously, for every woman who suffers a pulmonary embolism and actually dies, there are many more women who have a pulmonary embolism and do not die. So the morbidity statistics mirror these mortality statistics.
The bottom line: Tier 1 birth control (the LARCs) is the safest and most effective form of birth control and also has lowest rate of patient dissatisfaction, with the fewest side effects and highest continuation rates.
But what about cost?
While it is true that the upfront cost of a Tier 1 method is higher (ranging from $600-$800), the cost over time is much less. Popularly prescribed birth control pills cost up to $135 per month, while the cheapest pills are still around $20 per month. So just based on price, a LARC may pay for itself in as little as 6 months. Even with the cheapest choices, the three year methods pay for themselves in 30 months and the 5 and 10 year options pay for themselves in 3 years. Still, the real cost savings comes in the form of reduced costs of unintended pregnancies. Remember, 38% of women will become pregnant over 5 years with Tier 2 birth control versus less than 1% with a Tier 1 method.
So why should we use anything other than Tier 1 birth control?
Undoubtedly, the leading reason why women do not choose Tier 1 options is a lack of education and good counseling. The US lags behind the rest of the world in adoption of LARCs. Many primary care providers do not offer LARCs in their offices and hesitate to refer the patient elsewhere. The majority of providers do not adequately counsel women about the options. Even when patients are counseled appropriately, it is sometimes difficult to overcome negative information about LARCs found on social media, much of which is promoted by product liability attorneys seeking to solicit dissatisfied patients. It would be interesting to know how many women who have not selected LARCs – due to fear promoted by attorneys – have gone on to be harmed by their chosen birth control. Surely, the number of unintended pregnancies must be in the millions.
Still, there are some reasons why women might be better off with Tier 2 birth control choices. The suppression of the ovarian hormonal cycle might benefit them in ways beyond birth control, such as suppression and treatment of ovarian cysts, endometriosis, adenomyosis, dysmenorrhea, etc. The patient might have better control of acne or treatment of symptoms of PMS or PMDD. These “fringe benefits” of systemic hormonal contraception should be carefully weighed against the risk of unintended pregnancy with Tier 2 choices, and patients should make a truly informed decision.
Some patients might, for example, choose to use an IUD to prevent pregnancy while also using a birth control pill treat endometriosis (usually, there is no reason not do this). Another woman, however, who is planning a pregnancy soon anyway, and who wouldn’t be overly upset about a pregnancy, might choose just to use an OCP. Yet it is irresponsible if we give a 17-year-old, who seeks care for birth control to prevent pregnancy, anything other than Tier 1 birth control. Every time I place a LARC in a teenager, I think to myself that she will now likely graduate high school because I helped her make a good choice. This single act has a more profound impact on her life as a whole than almost anything else a physician can do.
Birth Control Comparison
Apart from failure rates, let’s look at the pros, cons, and contraindications of each birth control choice individually.
Nexplanon
Pros
- Highly effective for up to 3 years (likely the most effective form of female birth control, though a slightly lower continuation rate compared to IUDs)
- Preconceptual method (important to many patients)
- Reduced risk of endometrial cancer
- Effective for menorrhagia
- Nexplanon is radio-opaque
Cons
- Varying effects on ovulation (initially tends to inhibit ovulation but later does not; potentially changing effects on bleeding, ovarian cysts, etc.)
- Potential abnormal bleeding (most common cause of discontinuation)
- Potentially painful insertion and removal (though on the whole is very well tolerated when done correctly)
Contraindications
- Current breast cancer
- Severe cirrhosis or liver tumors
ParaGard
Pros
- Effective for at least 10 years
- Prevents fertilization
- No increased risk of PID
- No risk of infertility
- Cost-effective over time
- Highly effective, safe
- Completely non-hormonal
Cons
- Initially expensive
- May require referral
- Invasive; more painful to insert than Mirena or Skyla
- Does not diminish bleeding and, in fact, may increase troublesome bleeding
- Less effective than Mirena/Skyla
Contraindications
- Current pregnancy
- Current pelvic infection
- Pelvic tuberculosis
- Unexplained abnormal uterine bleeding
- Malignant gestational trophoblastic disease
- Untreated cervical or endometrial cancer
- Fibroids or anatomy abnormalities which distort the canal
- Wilson’s disease
Mirena
Pros
- Effective for at least 5 years
- Prevents fertilization
- Effectively treats abnormal uterine bleeding (it is the most effective non-surgical treatment for AUB)
- Protects against endometrial cancer
- No increased risk of PID (likely decreases the risk once placed)
- No risk of infertility
- Cost-effective over time
- Highly effective, safe
- Highest rate of patient satisfaction
- Lowest risk of death
- Little systemic effects
- Few contraindications
- No need for compliance
- Rapidly reversible
Cons
- Initially expensive
- May require referral
- Invasive
Contraindications
- Same as for ParaGard plus current breast cancer
Skyla
Pros
- Effective for at least 3 years
- Prevents fertilization
- No increased risk of PID
- No risk of infertility
- Cost-effective over time
- Highly effective, safe
- Highest patient satisfaction (even among adolescents)
- Lowest risk of death
- Smaller, easier to insert than other IUDs for women who have not had children
- Little systemic effects
- Few contraindications
- No need for compliance
- Rapidly reversible
Cons
- Initially expensive
- May require referral
- Invasive
- Less effect on abnormal uterine bleeding as compared to Mirena
Contraindications
- Same as for Mirena
Oral Contraceptive Pills (combination of estrogen and a progestogen)
Pros
- Noninvasive
- Easy to prescribe
- May have non-contraceptive benefits (“fringe benefits”)
- May be used to control timing of menses
- May be used as Emergency Contraception
- Reduced risk of endometrial and ovarian cancers
Cons
- 8.4% actual failure rate
- Side effects and resulting noncompliance, high rate of discontinuation
- Multiple drug interactions
- Multiple contraindications
- Increased risk of VTE
- Increased risk of MI in smokers > 35
- Increased risk of stroke in women with migraines
Contraindications
- Known thrombogenic mutations
- Prior thromboembolic event
- Cerebrovascular or coronary artery disease
- Uncontrolled hypertension
- Migraines with aura (any age)
- Migraines (over age 35)
- Diabetes with vascular complications
- Smoking (over age 35)
- Known or suspected breast cancer
- History of or known or suspected estrogen-dependent neoplasia
- Undiagnosed abnormal uterine bleeding
- Benign or malignant liver tumors, acute liver disease, liver failure
- Known or suspected pregnancy
- History of gastric bypass (pills only)
- Use of protease inhibitors, anticonvulsants, or lamotrigine alone, rifampin
- Less than 3 weeks postpartum
- Major surgery with prolonged immobilization
- Antiphospholipid antibody syndrome
Patch/Vaginal Ring (combination of estrogen and progestogen)
Pros
- Same as for OCPs
- May increase method compliance
Cons
- Same as OCPs
- Failure rates do not appear to be lower than with OCPs
- High absorbed estrogen with Patch
- Ring requires vaginal insertion and removal (which some patients do not like)
Contraindications
- Same as with OCPs except may use in women with history of gastric bypass
Depo-Provera
Pros
- Highly effective if patient is compliant
- Reduced risk of EM CA
- Effective for menorrhagia
- May raise seizure threshold
Cons
- Actual failure rate is around 6% due to noncompliance (largely due to side effects)
- Doubles risk of breast cancer
- Potential for irregular bleeding
- Weight gain
- Up to 22 month return to fertility
- Increased acne, hair loss
- 3.6x risk of thromboembolism
- May exacerbate depression
- Bone demineralization
Contraindications
- Current or history of breast cancer
- Diabetes with vascular disease
- Uncontrolled hypertension
- Ischemic heart disease
- Severe cirrhosis or liver tumors
- History of past or current CVA
I have not included in this list the progestin-only pill. In general, the progestin-only pill is less effective than combined OCPs and is typically given to breastfeeding mothers. This practice is based upon the flawed ideas that breastfeeding is a contraindication to use of OCPs or that they will produce less breast milk volume if used. Neither of these statements are true. These myths have been repudiated many times, yet the practice continues. For more information, here is a recent randomized trial.
I have also not included Tier 3 choices. Tier 3 choices are often selected for one of three reasons: other methods are not applicable due to presence of contraindications, previous negative side effects with birth control, or religious reasons. In general, the Tier 3 methods have high failure rates and high dissatisfaction rates. The one benefit, of course, is the prevention of STIs with condoms.
Most patients will choose a non-Tier 3 method with appropriate counseling. It’s hard to imagine a patient for whom all Tier 1 and Tier 2 methods of birth control are contraindicated. Many patients have had very negative side effects with birth control, but usually there is an alternate choice, which avoids the undesired side effect. Patients often would like to avoid methods of birth control that potentially interfere with the implantation of a conceptus. But this concern, too, is often mitigated with education about pre-conceptual methods (like the Nexplanon or IUDs).
How do I pick an OCP?
The lucrative marketplace of birth control pills is confusing. Provider preferences for prescribing pills are heavily influenced by marketing or anecdotal experiences. A lot of misinformation affects prescribing patterns. In general, prescription of OCPs should be based on cost, with changes to more expensive formulations based on side effects. No evidence exists that any particular OCPs is more effective than another. However, OCPs vary in the amount of estrogen they contain, how many days of hormones they have, and the type and amount of progesterone in the formulation. Some pills change the amounts of hormones during the cycle. Here are some important characteristics:
Phase
- Monophasic
- Most OCPs are monophasic, meaning that they contain the same amount of estrogen and progestin in every active pill.
- Biphasic
- These pills contain the same amount of estrogen in each active pill, but the amount of the progestin varies, usually changing twice.
- Triphasic
- Depending upon the brand, triphasic pills may change both the estrogen and the progestin throughout the month, or change the progestin only three times with three different doses (e.g. Ortho Tri-cyclen Lo).
Which phase should I pick? The evidence indicates that monophasic pills are usually the best choice (here and here). Bi- and triphasic pills do not offer any advantages and may lead to more side effects, and usually more cost. The original intent of lowering the amount of hormone (and thus limiting the total amount of hormone exposure) has largely been replaced with modern, low dose pills.
Cycle Design
- 21/7
- When OCPs were first developed in the 1960s, consumer marketing data indicated that women “wanted” to have periods. So pills were designed to create “a period,” with 21 days of active hormone, then a withdrawal time of 7 days during which bleeding would occur. There was never any scientific or health reason behind this. Most pills (and nearly all generic pills) are designed this way. Since the beginning, gynecologists have used 21/7 pills in different ways (usually just skipping the placebo pills) to treat conditions like endometriosis, dysmenorrhea, etc. More recently designed pills have sought to shorten or eliminate menses, as well as symptoms like PMS and PMDD.
- 24/4
- These pills offer 24 days of hormones with only four placebo days, thus shortening menses and reducing PMS/PMDD symptoms.
- 24/26/4/2
- Only one pill, Lo Loestrin, offers 26 days of estrogen and 24 days of progestin (with two estrogen free days and four progestin free days) with the goal of producing light to absent menses and eliminating PMS/PMDD symptoms while reducing total estrogen exposure.
- 84/7
- These pills are designed to give four withdrawal bleeds per year.
Note that virtually any hormonal preparation can safely be used to provide continuous hormonal suppression. For example, patients can skip the placebo pills of any of these preparations. They can also use the vaginal ring for four weeks, then replace it with another (rather than three weeks with a week off) or use the patch every week without an off-week.
If the intent of prescribing is only for contraception, then using a 21/7 pill (which is less costly) makes sense. However, if the desire is to treat conditions like abnormal bleeding, menstrual-related anemia, dysmenorrhea, pelvic pain, endometriosis, etc., then an extended or continuous cycle preparation is desirable.
Amount of Estrogen
All OCPs contain ethinyl estradiol, but the amount varies from a low of 10 mcg (available only in Lo Loestrin) to a high of 50 mcg. The first birth control pills in the 1960s had more than 100 mcg. The most commonly prescribed dose today is 20 mcg, though the least expensive generics have 35 mcg. Most side effects are linked to the amount of estrogen in the pill, as well as complications like blood clots. Therefore, in most cases, it makes sense to use a lower dose pill. Many generic 21/7 pills are available for a relatively low cost which contain only 20 mcg of estrogen. There is a considerable price difference between the one 10 mcg pill on the market and the less expensive 20 mcg generic pills (a difference of over $100 a month). In most cases, cost-consciousness should prevail.
Type of Progestin
There are several types of progestins available in birth control formulations. In theory, pills with higher progestational activity are associated with less abnormal bleeding and higher rates of anovulation. Pills with lower androgenic activity typically are better for symptoms like acne but perhaps worse for symptoms like decreased libido. In practice, there is very little real observable differences based on the type of progestin.
- Desogestrel
- Higher progestational activity, less androgenic
- Examples OCPs: Apri, Desogen, Mircette, Ortho-Cept, Reclipsen
- Drospirenone
- Very low androgenic activity (useful for PCOS, acne, etc.)
- Examples OCPs: Ocella, Yasmin, Yaz, Beyaz, Gianvi
- Ethynodiol Diacetate
- Medium progestational activity
- Examples OCPs: Demulen, Zovia
- Levonorgestrel
- High progestational activity, higher androgenic activity, most commonly used progestin
- Example Emergency Contraceptives: Plan B, Plan B One Step, Next Choice
- Examples OCPs: Alesse, Aviane, Lessina, Levlen, Levora, Lutera, Portia, Sronyx, Enpresse, Levlite, Tri-Levlen, Triphasil, Trivora, Jolessa, LoSeasonique, Quasense, Seasonale, Seasonique
- Non-pill Methods: Mirena, Skyla
- Norethindrone
- Low progestational activity, higher androgenic activity, slight estrogenic effect
- Example Minipills: Aygestin, Camila, Errin, Jolivette, Nor-QD, Nora-Be, Ortho Micronor
- Examples OCPs: Femcon Fe, Jenest-28, Junel, Loestrin, Microgestin, Modicon, Necon, Ortho-Novum, Ovcon 35, Tilia FE, Estrostep
- Norgestimate
- High progestational activity, lower androgenic activity, slight estrogenic effect
- Examples OCPs: Mononessa, Ortho Cyclen, Previfem, Sprintec, Ortho Tri-Cyclen, Ortho Tri-Cyclen Lo, Tri-Previfem, Tri-Sprintec, Trinessa
- Non-pill Methods: Ortho Evra (the Patch)
- Norgestrel
- High progestational activity, lower androgenic activity, slight estrogenic effect
- Examples OCPs: Cryselle 28, Low-Ogestrel, Ogestrel, Ovral, Lo/Ovral
- Etonogestrel
- Non-pill Methods: NuvaRing, Nexplanon
So how do I pick an OCP?
- If it is for birth control only, and for some strange reason the patient doesn’t want a Tier 1 option, use an inexpensive 20 mcg pill (generics of Alesse or Lutera for example).
- If it is to treat acne or PCOS, consider a pill that contains drospirenone.
- If it is to treat endometriosis, pelvic pain, abnormal bleeding, or dysmenorrhea, consider an extended release or continuous release pill (such as Lo Loestrin, Minastrin, or the generics of Seasonique).
- If a patient has androgenic side effects (like acne), consider a pill with less androgenic activity.
- If a patient has hypo-androgenic side effects (like decreased libido), consider a pill with more androgenic activity.
- If a patient has breakthrough bleeding, consider a pill with higher progestational selectivity (like norgestimate or levonorgestrel).
- If a patient has headaches or nausea, consider a pill with less estrogen (like Lo Loestrin).
Other tips:
- Don’t forget that patients need 13 packs per year. So prescribe one pack plus 12 (not 11!) refills.
- Don’t focus on adding estrogen as the solution to breakthrough bleeding; the ratio of estrogen to progestin and the type of progestin is more important. Often in the face of irregular bleeding, a physician might switch to an older pill like Ortho Cyclen because of the increased estrogen; but in actuality, it was switching to norgestimate that made the difference.
The Bottom Line
One of the most important indicators of quality among Ob/Gyns is how often they utilize Tier 1 birth control. It is hard to make an argument why we should not use the most effect, lowest cost, least harmful, most satisfying form of birth control. Be a LARC advocate!
For More Information
Absolute and Relative Contraindications of Birth Control Chart
CDC Recommendations for Contraceptive Use
Failure Rates Over Time: Interactive Graph
Reproductive Health Access Project
CDC Contraceptive Guidance for Health Care Providers