The modern chief resident in Ob/Gyn (and I am certain in other specialities) has few characteristics in common with the role of a chief resident in decades past. This change, like most changes, is both good and bad. Most chief residents today are not really “chiefs” in any meaningful sense of the word, but are rather just last-year residents, still learning basic and intermediate skills, with a few administrative responsibilities. Those administrative responsibilities may or may not include things like making the call schedule, the rotation schedule, assigning residents to various tasks and conferences, and maybe dealing with vacation requests.
This level of “responsibility” is akin to the level of responsibility a fast food store manager might have, without concerns like payroll, hiring and firing, conflict resolution, etc. In other words, it’s not real responsibility and it rarely comes with real authority. A program director (or administrative secretary) is always ready to veto or change anything he might not like about the chief resident’s decision.
Several events have conspired to change the landscape for chief residents. Due to billing and liability concerns, chief residents are given far less autonomy and responsibility than in the past. Virtually every meaningful decision nowadays is made by the attending physician. This may or may not be a good thing in terms of patient quality (it probably depends on how good the attending is), but it is a devastating thing for the chief resident, who no longer feels a real sense of responsibility for the decisions she is making (while still having a safety net). Most often, the first time a physician feels ultimately responsible for the patient is during the first year of practice post-residency, but by that point the safety net is usually gone and the cost of failure is much higher.
Residency work hour restrictions, coupled with a declining volume of surgical cases, have made the last year of residency more important in terms of learning how to do more advanced procedures or becoming more skillful at basic procedures. In Ob/Gyn, most residents today graduate unable to safely perform a vaginal hysterectomy and several other procedures independently, according to a 2015 study of Fellowship Directors. They found that,
- Among incoming oncology fellows:
- Only 44% could independently perform a hysterectomy,
- Only 48% could operate independently without the attending present for 30 minutes of a major procedure.
- Only 52% could appropriately pack the bowel for pelvic surgery.
- Only 80% could perform a LEEP correctly.
- Only 68% could perform a laparoscopic BSO independently.
- Only 52% of the fellows were able to take general gynecology call without supervision.
- Among incoming Urogynecology fellows:
- Only 20% of incoming fellows could independently perform a vaginal hysterectomy.
- Only 17% could perform a vaginal bilateral salpingo-oophorectomy.
- Only 23% could perform an anterior colporrhaphy.
- Only 30% could perform a posterior colporrhaphy.
- Only 20% were able to perform transvaginal or transobturator taping.
- Only 27% were able to fix a cystotomy to the dome of the bladder.
- Among MFM fellows:
- Only 72% of incoming fellows could independently perform a vacuum-assisted vaginal delivery.
- Only 83% could repair a third-degree laceration.
- Only 67% could perform a complicated cesarean delivery.
- Only 67% felt that the fellow could place an O’Leary stitch.
- Only 39% of respondents felt that fellows could recognize normal anatomy and only 17% felt that the fellow could identify major genetic or anatomic abnormalities.
- Only 31% of the incoming fellows were rated as competent to perform forceps deliveries.
- Among REI fellows:
- Only 18% of incoming fellows could independently perform a laparoscopic hysterectomy.
- Only 31% could safely perform an abdominal myomectomy.
- Only 35% could perform a hysteroscopic myomectomy.
- Only 12% could perform a laparoscopic myomectomy.
- Only 42% could perform a hysteroscopic lysis of adhesions.
- Only 65% could perform a laparoscopic ovarian cystectomy.
In theory, these graduates entering fellowship training are the crème de la crème. If they are (I have my doubts), then our speciality is in trouble. If the numbers are this bad for graduates entering advanced training fellowships, imagine how bad they are for the average chief resident beginning the last year of training.
Since the chief residents are still incompetent to do many procedures, this creates a situation where the chiefs “steal” the cases from juniors, which perpetuates the vicious cycle of unprepared chief residents. The juniors will enter their chief years woefully unprepared, and worse, the role of chief resident as teacher is all but destroyed as they struggle just to gain some glimmer of competency for themselves.
Teaching is perhaps the most important role of a chief resident (or at least it should be). I learned a lot during the first 20 or so hysterectomies I did, but I learned a lot more during the first 10 that I taught. Even today, I usually learn far more by first-assisting someone than by doing the actual procedure. But a chief resident, who is still not far enough along the learning curve to start teaching, or, more likely, who has not developed enough self-efficacy to give up the case to a junior and teach her how to do it, cannot develop competency because competency and mastery ultimately comes from teaching.
Unfortunately, today, the junior faculty have actually assumed the role of chief resident, and their own competencies and sense of self-efficacy is stuck in that role unless they are lucky enough to grow out of it. An incompetent chief resident who goes into a non-academic practice may never have the opportunity to complete his education through teaching.
The Cognitive Apprenticeship Theory describes the process of a master of a skill teaching a novice apprentice. Various teaching methods can be used during such an apprenticeship. In residency training, we typically see modeling and coaching. In modeling, the apprentice learns from watching the master, and then in coaching, the master gives feedback to the novice while the novice attempts the different skills. There are other methods that are often neglected in modern residency teaching which are necessary to develop mastery.
For example, exploration allows the novice to problem solve on her own; in today’s environment of almost too much supervision and zero tolerance for any type of failure, this important method of education is almost never appropriately utilized.
Another method, articulation, is also not fully utilized. Articulation involves the novice articulating their knowledge, reasoning, and problem-solving in an effort to force synthesis and allow the novice to have knowledge gaps or reasoning errors highlighted so that they can be corrected. In medical education, the role of the novice (the resident, medical student, junior faculty member) in teaching is where most articulation occurs. Depriving the chief resident of the role of teaching junior residents deprives them of this important learning method. I should note that the depth of teaching and the perceived importance of the teaching matters. If a chief resident, for example, is tasked with teaching a junior resident or medical student only basic and non-ambiguous skills and information, rather than complex and nuanced decision making, data interpretation, and advanced skills, then the chief resident is not really benefitting.
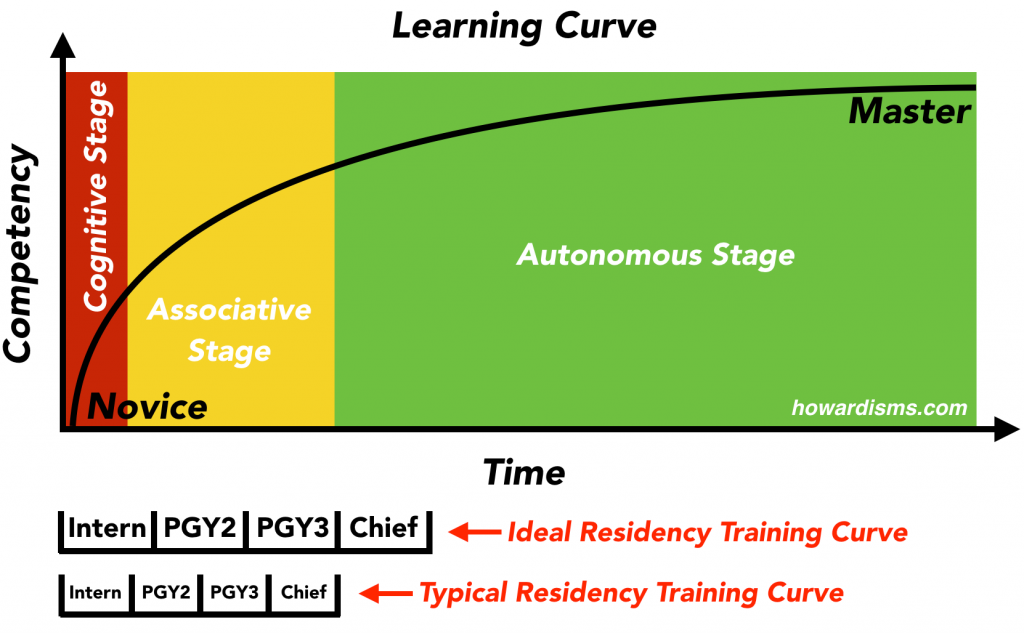
Most authors recognize that the Cognitive Apprenticeship Theory proceeds in defined stages. The Fitts and Posner three stages model is frequently applied to this. The three stages are the cognitive stage, associative stage, and autonomous stage.
In the cognitive stage, novices learn the theory of the skill. In the associative stage, they practice the skill and learn from mistakes and misinterpretations while the salient and most important points of the skill are reinforced by the master. In the autonomous stage, learners are skilled enough to practice the skill independently and they possess the requisite skills that allow them to continue to learn from their practice until they become an expert. In practical terms, this may mean reading about vaginal hysterectomy and watching videos and observing and assisting in surgeries during the cognitive stage; then performing vaginal hysterectomies with a teaching assistant who gives good feedback during the associative stage; and lastly, assisting learners with vaginal hysterectomies or performing them independently without a teaching assistant (no attending) during the autonomous stage.
Most residents graduate from residency without ever starting into the autonomous stage. Chief residents may still be early in the associative stage for skills like vaginal hysterectomy at the time they graduate. Because they don’t reach the autonomous stage while still supervised, they may not learn the skills needed to continue to learn from their own experiences and therefore may never advance to mastery. They also often lack the necessary skills for lifelong learning and independent critical thinking necessary to stay up to date during their careers.
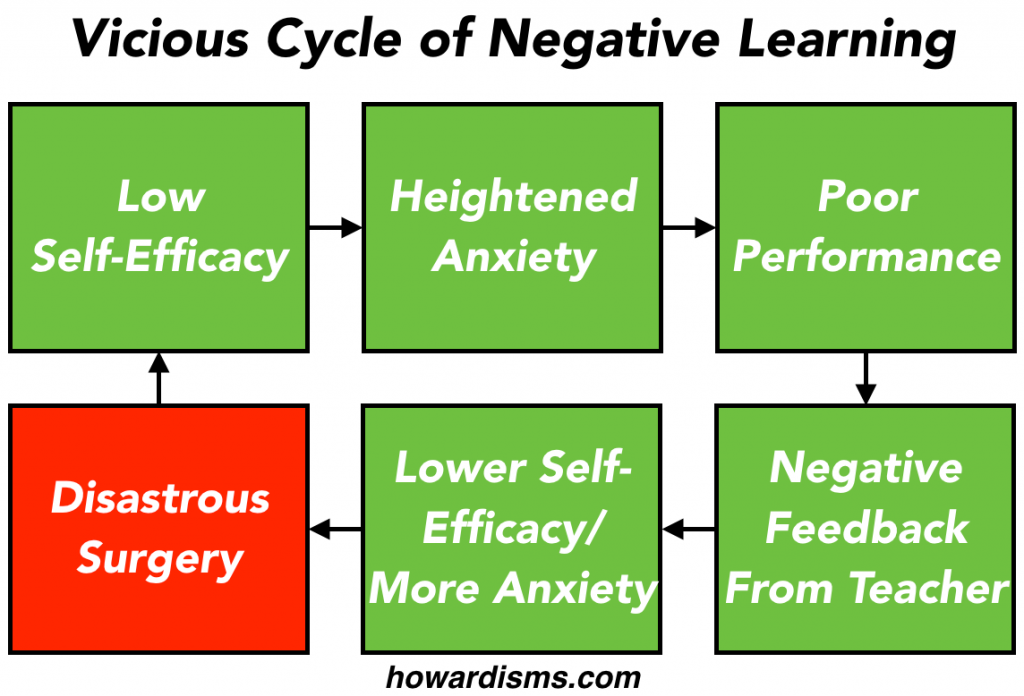
Self-efficacy is a measure of how much one believes that she is able to complete tasks or reach goals or work through problems. Interns have a low degree of self-efficacy, at least related to medical problems. In theory, a graduating resident, ready for independent practice, would have a relatively high degree of self-efficacy. This self-efficacy is necessary to progress through the autonomous stage and advance towards mastery. For people with low self-efficacy, obstacles seem larger than they really are, tasks seem more difficult than they should, and adversity quickly leads to giving up and failure. Physicians with low self-efficacy lack resiliency, and as such suffer from more anxiety and depression. Because surgeons with low self-efficacy believe that a task (a surgery) is harder than it actually is, their performance suffers and the surgery becomes more difficult, leading to a vicious cycle of prophetic self-fulfillment. Albert Bandura identified four factors that affect self-efficacy: experience, modeling, social persuasion, and physiological factors.
Experience is a major promoter of self-efficacy (either positively or negatively). Achieving expertise (in anything really) helps develop self-efficacy. Specifically, in a surgical specialty, gaining expertise in a surgical procedure fuels self-efficacy. Residents who graduate without expertise obviously have poorer self-efficacy as a result. I always like to ask learners to tell me something they are good at, something that they can teach me. The topic doesn’t really matter because I am tricking them into feeling a heightened sense of self-efficacy and accomplishment that they can translate into the current task or educational goal.
Modeling is best expressed as the feeling that “if he can do it then so can I.” Once Roger Bannister finally broke the four-minute mile threshold, his record lasted just 46 days. Four minute miles soon became routine for top runners. The self-efficacy of every other sprinter in the world was raised by Bannister’s feat. Bannister, by the way, was a medical resident at the time he broke four minutes (he actually had been at work at a London hospital that morning). One of the negatives of the current modeling in residency programs is that most residents rarely see surgery done well. With less accomplished senior residents, and junior faculty who lack self-efficacy, surgeries seem far more difficult that they should be. Hysterectomies that should take 20-30 minutes instead take 2-3 hours; cesareans that should last 10-20 minutes instead take 1-2 hours. Modeling as a means of self-efficacy development is largely missing from current residency training. If the chief resident struggles miserably to do a hysterectomy, what hope does the junior resident have? When the resident leaves the case feeling defeated and intimidated, self-efficacy drops dramatically. It is the attending physician’s responsibility to ensure that this never happens.
Social persuasion is related to the type and amount of encouragement or discouragement that a person receives. Encouragement typically promotes higher self-efficacy, while discouragement generally promotes lower self-efficacy. As you might guess, most of residency training is focused on negative feedback and therefore discouragement leading to lower self-efficacy. We have morbidity and mortality conferences to scorn failure rather than conferences that reward successes. We always focus on what could have been done better rather than on what went well. Good teachers understand this instinctively. We don’t need to undermine self-efficacy by sharp criticism; rather we need to build on successes. No resident does every task perfectly. We should try to positively reinforce what has been done well rather than constantly point out deficiencies. This is an important part of the associative stage of the cognitive apprenticeship model; the good things and important steps are to be reinforced, not the negatives. The greatest role of a teacher is to encourage.
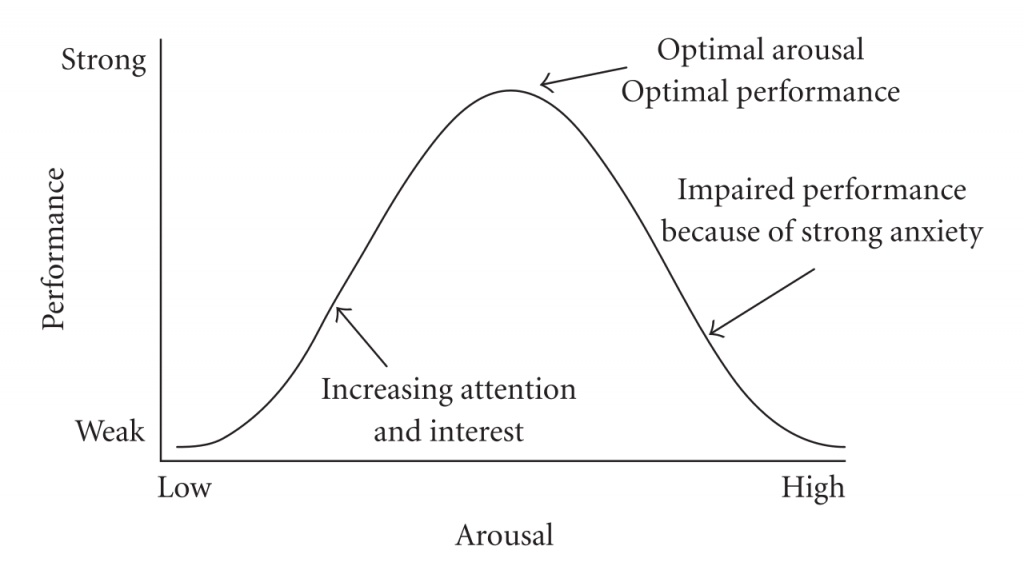
The physiological factors that affect self-efficacy relate to our stress response. If a situation makes us nervous and anxious, the physiological response to this stress will tend to lower our self-efficacy and make us consequently underperform. A good teaching environment is relatively stress free. Does that sound like most residency programs? The Yerkes-Dodson law describes this behavior:
Anxiety management of learners (and surgeons) is critical to effective education (and successful surgeries).
Self-efficacy is something that should be continuously fostered and promoted in residency training (and all other training). Most chief residents today have very little self-efficacy.
What are some solutions?
- Chief residents should enter the autonomous stage of the apprenticeship during their chief year (not after graduation).
- They should predominantly teach procedures and skills to junior learners, taking over only the most difficult cases.
- They should have real responsibility and authority for patient care and administrative tasks.
- They should be allowed a lot of leeway and liberty to experiment and an opportunity to learn from their missteps (this doesn’t have to compromise patient care at all).
- They should be made to feel the safety net of the attending physicians slowly and progressively slip away (though the safety net never need actually be removed).
- They should be allowed to practice mostly independently and be allowed to problem solve, analyze data, and make complex decisions (and make mistakes).
None of this means that they shouldn’t be supervised. But it does mean that attending physicians should sign off on their management plans at the last stage unless there is a very important reason not to. In essence, the chief resident should be serving as a junior faculty member.
Consider these two examples:
A patient comes to triage to be evaluated. The junior resident assesses the patient and tells the chief resident. The chief resident presents the patient to the attending physician.
- In one scenario, the chief resident then presents the data (the history, physical, etc.) to the attending physician and the attending then makes a decision (“Okay, sounds like she needs to be admitted. Start pit and penicillin).
- In another scenario, the chief presents the data to the attending and then makes a decision and outlines a plan of care (“So I’m going to admit her and start pit and penicillin for GBS”).
This subtle distinction is all the difference in the world in effective education. The attending may ask about the chief’s thought process and may teach a general principle related to the problem, but unless the assessment and plan are completely off the reservation, the attending physician should just approve the plan. This promotes the chief’s self-efficacy, her sense of responsibility, the respect for the chief by the junior residents, and gives the attending physician an opportunity to assess reasoning and decision making abilities for the chief which may need to be fine-tuned. In turn the chief resident should do most of the teaching for the junior staff.
In surgery, whenever possible, the model should similarly be that the chief resident teaches and assists the junior resident. I honestly believe that it requires as much if not more skill to be a good assistant as it does to be a good surgeon. True mastery of surgery comes from the ability to teach and explain every step to a novice. Many residents graduate not understanding many of the steps of a surgery or their importance, but rather they just practice mimicry of surgeries they have seen, aping each step. This is the difference between a parrot and a person: both can say words, but the parrot doesn’t know what they mean or when they should and shouldn’t say them. A lot of practicing Ob/Gyns and surgeons are mere parrots in the operating room.
This also means that residents need earlier exposure in the operating room than they get in many programs. The goal should be for residents to be leaving the third year at the place where fourth year residents are leaving now. We need to regain a year, and we need to do so in the face of shortened work days and fewer cases. Undoubtedly, simulation and technology will need to serve a larger and larger role in developed core skills for trainees so that each surgical opportunity becomes more valuable (and safer).
A lack of self-efficacy among chief residents and faculty also promotes a negative work environment for everyone. Most bullying behaviors in the workplace are driven by the low self-esteem of the bully. Chief residents are encouraged to be selfish (steal cases) and hostile to juniors as they deal with their own negative feedback, anxieties, and fears as they come closer to graduation not knowing what they are doing. Culture is important, and bullying and negative treatment should never happen.
It’s time to end this negative cycle.